Ethnography Summary
Grace Hasbun and Victoria Velasquez interviewed Debra Stanley, the founder and manager of Imani Unidad. Debra was in company of Bayay, Peer to Peer group coordinator, and Andy, intern.

^ Debra’s contagious laughter
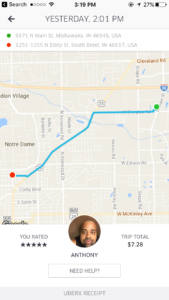
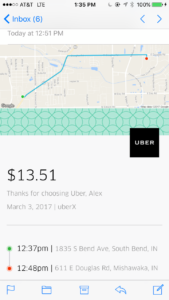
Date: March 3, 2017
Type: Expert Interview
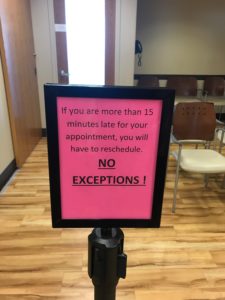
Location: 914 Lincoln Way West, Colfax Cultural Center, first floor
Team participants: Victoria Velazques & Grace Hasbun
User Characteristics: Female, age 50s, 60s
Passionate. Founder and manager of Imani Unidad, a charitable, non-profit organization whose goal is to provide community education and advocacy efforts to its members, who are strongly stigmatized by both society and themselves.
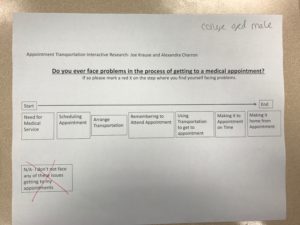
GH and VV interviewed Debra concerning the main issues Imani Unidad addresses. Information involved the organization’s mission, goals, structure, members, and services. Focusing on what Debra believes is the main problems or barriers the members encounter when interacting with the community. Specifically, barriers involving housing and employment due to society’s stigmas.
Members of Imani Unidad (target users): The organization includes HIV/AIDS and/or formerly incarcerated individuals, Individuals with substance abuse history.
Personal Development Portion: Personal Development Portion helps reduce the stigmas that are self-imposed by the members. Imani Unidad unlike other agencies focuses on the internal development piece of the individuals and the community education about their situation. This focus is due to a gap Debra saw in the other regular services, whose focus is merely on external re-installation. The organization includes Individual and Group Level Services for Personal Development. This is an essential piece for HIV+, former incarcerated, and/or individuals with substance abuse; this service is “very much tailored to the individual, and our whole goal is to help them get to the place where they become their own best advocate”.
Community Education Portion: The Community Education Portion seeks to help members against societal stigmas and barriers for to HIV+, former incarcerated, and/or individuals with substance abuse issues. Including City Council, County Council, Landlords, Employers. Who pose barriers and stigmas towards the individuals.
Top 3 learnings:
(1) Imani Unidad offers personal development services that are tailored to the individual’s needs and to impulse the personal desires of improving. Also, it allow them to grow on the community/group/peer support.
(2) The community education part requires a lot of work, considering the current situation stigmatization. Specifically, for the target group it is hard to find housing, employment and even healthcare. Thus, it becomes a cyclical/vicious cycle that leads them to falling again in substance abuse, and/or homelessness, and not able to personally develop.
(3) At this juncture Debra and Imani Unidad are trying to formulate the “talking points” that speak specifically to the community. Formulate what exactly are the barriers/situations, stigmas/discrimination, and laws/corruption that are currently negatively impacting both Imani Unidad members and society as a whole.
Differentiate between the believed vs actual consequences/results of these barriers built.
Key Insight: Imani Unidad deals with marginalized people. Their goal is making sure that these individuals become their best advocates, and to educate the community so that they don’t build barriers that discriminate this group unnecessarily.
QUOTES
“We are the, what I consider, the personal development piece… allowing them to get to the place where they could become their own best advocate”
“…so it is very individualized, no box or pattern, and different people want different things, and that’s what we are all about.”
“Why are they (government officials) allowing substandard structures to exist..”
“you end up discriminating against people, unnecessarily”
“part of the education is trying to build people up”
(…topic: individuals speaking up for their rights…)
“There is always this fear that the adverse impact is going to be greater is I say something”
“This allows people who discriminate, even greater power over people”
“That’s why education with folks is so important; creating this sense of community and support… so they don’t have to feel so alone.”
Activities:
- Debra had arrived to SB 3 days before, arriving from California.
- Grace called Debra to confirm appointment, nice and welcoming she gave directions
- At the time of the meeting Debra was working in her office, and guided to a larger “meeting room” with Andy.
- Introduced Bayay and Andy
- Grace took pictures and recorded the conversation
Environment
- 12:00-1:30pm
- “meeting room” had bright, lively orange walls, and animal/forest paintings that students had painted as a service for Imani Unidad.
- Red brick buiding was a large and “antique”
- First floor, large room with long crocodile shaped carved wood.
Interactions:
- Individuals in the building guided Grace to Debra’s office
- Input and further insights from Bayay, Andy
- Debra was passionate, loud, and has a contagious laughter
Objects:
- Large table to sit around
- paper, pen, glasses
- Office room, with computers, many files
- GH and VV labtops
- Phone’s video camara
Users:
- Debra Stanley
- Bayay
- Andy
- Grace Hasbun
- Victoria Velazquez