Michael Murakami
As an accountant and economist by trade, the theological story I am most naturally drawn to is when Jesus calls upon Matthew the tax collector (soon to be St. Matthew, Patron Saint of Accountants) to join him in ministry. Jesus’ quote in Matthew 9:12, “It is not the healthy who need a doctor, but the sick”1 was always memorable; knowing that sinners (the sick) could be drawn into and saved in the church by Jesus (the doctor) comforted me. Yet in modern society, this initially metaphorical line now applies in a very literal sense: many regions of the United States, like rural communities, are populated with “sick” people who are unable to receive treatment for a variety of reasons, such as time, cost, and access.

Background on Rural Communities
Social determinants of health (SDoH) impact rural communities by decreasing the healthcare access and utilization of residents. Some of the most common SDoH in rural areas relate to lower levels of income, education, health-related infrastructure, and health literacy as well as other determinants such as race, ethnicity, sexual orientation, and environmental impacts.3
To exemplify the impact of a SDoH, Elisabeth Rosenthal describes in her piece, Paying till It Hurts: The $2.7 Trillion Medical Bill,4 how patients with lower incomes suffer because of rising costs and doctor-patient information asymmetry. The example she uses is colonoscopies, where it is shown that pricing is not equal nor well understood, even by doctors. However, even worse, because of the specialized knowledge of the medical field, patients typically do not understand what procedures or checkups most efficiently diagnose or aid their issues and are cornered into what doctors prescribe. The fundamental problem that results is that the motivations of doctors can be fueled by popular, but misguided medical beliefs (in this case, that colonoscopies are the best method for the early detection of GI issues) or lobbying of medical firms (more often seen in pharmaceuticals). In either case, low-income and low-access patients are most impacted by ineffective and unnecessary testing because they are least able to afford or access further care.
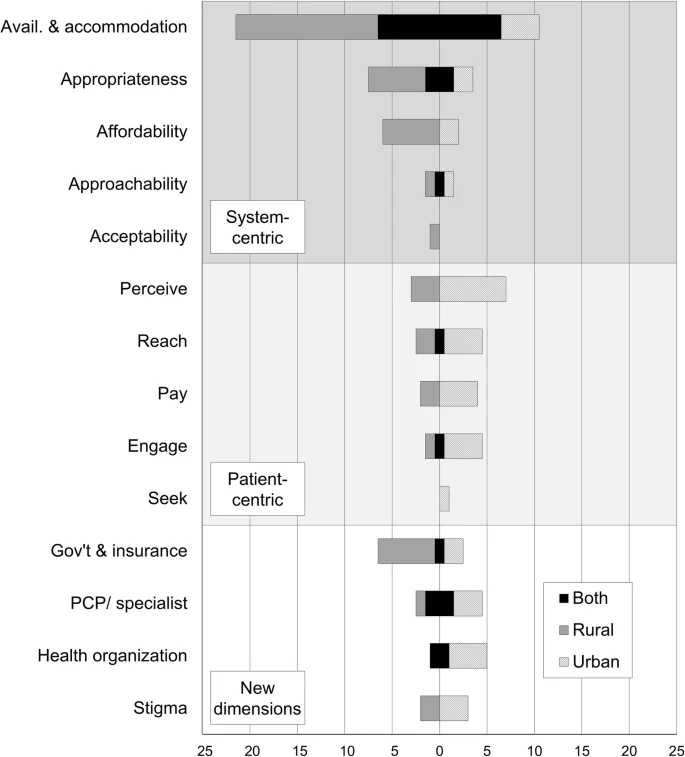
Beyond lower financial access and utilization of medical care, geography plays a critical role in physically limiting the access of rural patients from doctors. According to a study comparing rural and urban specialty healthcare access by Melissa Cyr et. al., both urban and rural areas struggle with the availability and accommodation of healthcare, although rural areas are considerably worse off (a problem compounded by additional limiting factors) as seen in the infographic below.5 Here, Cyr et. al. shows the existence of a variety of significant barriers to healthcare access in rural areas.
This dramatic difference in access and utilization tangibly impacts the quality of life and longevity for rural and poorer communities. In his piece, Inequality and the Health-Care System in the USA, Samuel Dickman explores the lower quality of life and shorter life expectancies for low-income patients. He explains that chronic and acute conditions alike have higher prevalence with declining income (which is correlatable strongly to rural communities) as well as considerably lower life expectancy.6 These results exemplify how the negative outcomes associated with SDoH decrease the quality of an already shortened life.
The Role of Rural Communities in the United States
With an understanding of the existence of disparities and deficiencies in healthcare from the above pieces, one may ask why only a small segment of society pushes for changes to the status quo. A common response draws upon economics in a resource-constrained game; proponents believe that the tradeoff of additional healthcare being invested in densely populated areas will help more people than in rural areas. This utilitarian stance, although logical on the surface, lacks consideration for the whole picture when further analyzed. To understand an unempathetic, economic argument in support of expanding rural healthcare, one must understand the role of rural, especially farming, communities in the United States. In rural America, approximately one out of ten workers are in industries such as agriculture, fishing, and hunting which, although decreasing over time, comprises a large portion of the community and nationwide production.7
Open market and even Keynesian economists may argue that we should help rural communities in order to directly strengthen our food source, therefore bettering society. This stance stems from a belief that farming communities (and other rural industries, however, farming is a clear example) will become more productive with increased average levels of health and health outcomes. Adam Smith points to this idea in The Wealth of Nations, the foundational text in support of capitalism and market economies. He describes how “no society can surely be flourishing and happy, of which the far greater part of the members are poor and miserable.”8 Even in a true capitalist market economy (which the United States is not), Smith argues that those rich in money and/or other goods will only live in a flourishing society by ensuring a respectable minimum living threshold for its members. In this case, the reward of a “flourishing” society results from the positive externalities associated with more efficient, healthier farmers who create more food for everyone. Uplifting rural farming communities’ healthcare resources and overcoming existing SDoH from this economic perspective is not an emotion-based decision but rather a net-positive sum game and an economically sensible choice.
Yet, this economic argument does not feel satisfying, even to an economist like myself. Instead of uplifting communities for their intrinsic value, this action derives its motivation from how it benefits me and my community. Rather, it may be beneficial to consider shifting the argument away from the expected net societal value of healthcare expansion and towards viewing farmers as intrinsically valuable and deserving of better health outcomes. For this view, we turn to Immanuel Kant, who describes how we must:
“Act in such a way that you treat humanity, whether in your own person or in the person of any other, never merely as a means to an end, but always at the same time as an end.”
Immanuel Kant, The Metaphysics of Morals9
Rethinking Rural Healthcare
Therefore, more than a means to efficient food production, one ought to look at the problem of rural healthcare from the lens of helping the communities in and of themselves. This empathetic call for improved rural medical access stems from the societal obligation to help create access to foundational resources to highlight the inherent and divine dignity of every person. The conversation thus returns to the ministry that Jesus called Matthew the tax collector to join.
Theologically, the societal obligation to assist others for their intrinsic value appears prior to the Gospel of Matthew in the Old Testament, for Proverbs 31: 8-9 declares that we must “Speak up for those who cannot speak for themselves, for the rights of all who are destitute. Speak up and judge fairly; defend the rights of the poor and needy.”10 It is not just for privileged communities to look down upon lower average health outcomes in rural communities. Much the opposite. We as members of a privileged section of society are each called upon in the fight to assist rural areas by creating new opportunities for financially and geographically feasible healthcare access.
From all of these ideas, we find the final conclusion. It does not matter whether rural communities are viewed as a means to resources for the rest of society or end in themselves, for healthcare is not and has never been a net-zero sum game. Rather, all perspectives understand the positive-sum nature of increased healthcare and better medical outcomes for rural communities. What implementing this solution looks like in real life is not in my wheelhouse, I am just an economist after all. But in this fight, all members of society should and ought to support actions that help rural communities overcome the SDoH that plague the status quo.
Works Cited
1) “Bible Gateway Passage: Matthew 9 – New International Version.” Bible Gateway, www.biblegateway.com/passage/?search=Matthew+9&version=NIV.
2) “The Calling of Saint Matthew.” Artble, Artble, 19 July 2017, www.artble.com/artists/caravaggio/paintings/the_calling_of_saint_matthew.
3) “Rural Health Information Hub.” Social Determinants of Health for Rural People Overview, www.ruralhealthinfo.org/topics/social-determinants-of-health.
4) Rosenthal, Elisabeth. “The $2.7 Trillion Medical Bill.” The New York Times, The New York Times, 1 June 2013, www.nytimes.com/2013/06/02/health/colonoscopies-explain-why-us-leads-the-world-in-health-expenditures.html.
5) Cyr, Melissa E., et al. “Access to Specialty Healthcare in Urban versus Rural US Populations: A Systematic Literature Review.” BMC Health Services Research, vol. 19, no. 1, 2019, doi:10.1186/s12913-019-4815-5.
6) Dickman, Samuel L, et al. “Inequality and the Health-Care System in the USA.” The Lancet, vol. 389, no. 10077, 2017, pp. 1431–1441., doi:10.1016/s0140-6736(17)30398-7.
7) Staff, America Counts. “More Work in Education and Health Care.” Census.gov, 15 Sept. 2022, www.census.gov/library/stories/2017/08/rural-economy-not-completely-dependent-on-farming.html.
8) Smith, Adam. The Wealth of Nations. Seven Treasures Publications, 2009.
9) Kant, Immanuel. The Metaphysics of Morals. Bobbs-Merrill Education, 1965.
10) “Bible Gateway Passage: Proverbs 31:8-9 – New International Version.” Bible Gateway, www.biblegateway.com/passage/?search=Proverbs+31%3A8-9&version=NIV.
