According to Vox, nearly 48 million Americans provide some form of informal care to an adult with either physical or mental health needs. My mother happens to be one of these people. She takes care of her mother–my grandmother–who has Alzheimer’s, and who is also physically unable to take care of herself. Family caregivers, like my mother, play a critical role in providing care and support to individuals who are unable to take care of themselves due to age, illness, or physical or mental disability. A challenge that many family caregivers have faced since the Covid-19 pandemic is the inability to take off work to be able to care for their loved ones, which puts caregivers in an unfair situation–to either provide less care or lose their job. Because of the time and extensive care that many older patients require, the commitment for family caregivers is immense. Fortunately enough, my mother happens to be one of the lucky ones.
Source: National Alliance for Caregiving (NAC)
According to the KFF reading, many family caregiving responsibilities (both before and after the pandemic) largely fall on women. More than one in ten women report they were caring for a family member who needed special assistance prior to the pandemic, and over one in ten women also report that they have new caregiving responsibilities as a result of the pandemic. As I think about my parents, my mother happens to have an older mother than my dad’s mother (she’s 84), so it makes sense that she is the one that has caregiving responsibilities. Thankfully, my dad’s mother is only 63 and father only 67 (both in very good physical shape), so I don’t foresee my dad having to take on the role of caregiver anytime soon. However, the findings about gender differences in caregiving was striking to me nonetheless.
Source: Unsplash
Since 2020, my mother has worked from home and our family relocated cities from New York City to Milwaukee, WI. Now, my mother is a short drive from the facility that my grandmother currently lives in. She is able to see her everyday and is constantly checking in on her, bringing her meals, and taking her to doctor’s appointments. However, she is not paid or compensated for the time, money, and care that she pours into my grandmother. My mother would do what she does whether she was paid or not, however it does significantly affect her everyday life. This kind of constant care can take a significant toll on caregivers’ physical, emotional, and mental health. Specifically, as my grandmother’s Alzheimer’s has progressed, my mom has experienced increased feelings of sadness, anxiety, and hopelessness when she visits my grandmother.
Source: MDPI
These kinds of feelings are common among caregivers and exposes the flaws in the American healthcare system that do not provide family caregivers with the proper help, resources, or money that they need to not only take care of their loved ones, but to take care of themselves in the process too. The lack of proper healthcare services and resources in the United States places a significant burden on family caregivers, who may struggle to provide the care that their loved ones need while also maintaining their own physical and mental health and well-being. Addressing these issues will require a comprehensive approach that addresses the systemic economic, social, and cultural barriers to accessing proper healthcare services and resources.
Source: Atlas
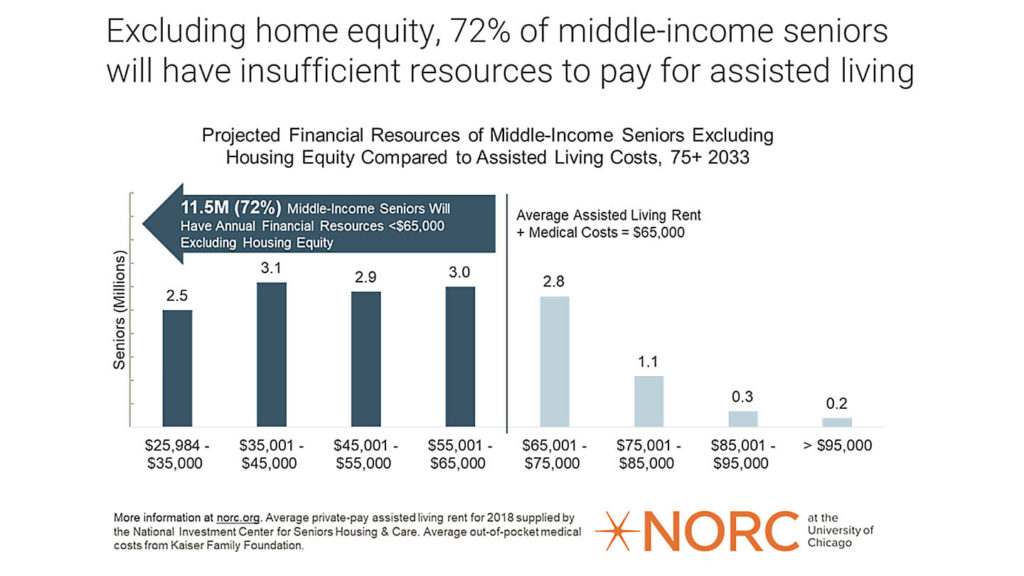
A topic that we did not discuss too much in depth in class, but directly relates to the healthcare system, unpaid family caregivers, and the inequalities that are exacerbated, is long-term care insurance. Privatized long-term care insurance is something that my grandmother was afforded after being a public school teacher in Wisconsin for nearly fifty years. In the 1960s, my grandmother and other teachers like her were not paid well, however in return she was provided with great health insurance, life insurance, and dental insurance. Even though the insurance at the time was great, because healthcare costs for the elderly in the United States have skyrocketed tremendously, her insurance only covers about half of her facility bill, which is $7,000 a month for a single room. My grandmother has recently moved into a shared room with another woman, with the cost being $3,000 less, so the insurance covers the entirety of the bill now. However, the cost for the facility that my grandmother lives in is still too steep for most Americans to pay, leaving them no option but to place their elderly loved ones into nursing homes–instead of homes with more comprehensive, tailored care such as assisted living or memory care facilities.
Source: McKnights Senior Living
The American healthcare system does not prioritize or protect its elderly population. One of the main issues is the high cost of healthcare, which is often unaffordable for those aged 65 and older that are living off of fixed incomes. Many elderly patients also struggle to access quality care because of their inability to be mobile. There is a significant lack of attention on preventative care for seniors, which can lead to more serious health issues down the line, as well as frequent instances of medical errors and misdiagnoses that can have devastating consequences for elderly patients. Reforms are needed in the American healthcare system to protect our elderly population. This could include policies that expand access to affordable care for seniors, provide more comprehensive coverage for preventative care, and implement stronger safeguards to prevent medical errors. Protecting the elderly is so important because they are a vulnerable group at higher risks for health issue, financial insecurity, and social isolation. They have contributed to the inner workings of society for decades, and deserve to be treated care. Their health and well-being is crucial for the overall functioning of society.
Sources
Alzheimer’s Association. (2022). What is Alzheimer’s Disease? Retrieved March 27, 2023, from https://www.alz.org/alzheimers-dementia/what-is-alzheimers.
Breijyeah, Z and Karaman, R. (2020). Comprehensive Review on Alzheimer’s Disease: Causes and Treatment. DMPI. Retrieved March 27, 2023, from https://www.mdpi.com/1420-3049/25/24/5789.
CAP. (2014). Reforms to Help Meet the Growing Demand for Long-Term Care Services. CAP. Retrieved March 27,2023, from https://www.americanprogress.org/article/reforms-to-help-meet-the-growing-demand-for-long-term-care-services/.
Courage, H. (2021, August 4). America isn’t taking care of caregivers. Vox. Retrieved March 27, 2023, from https://www.vox.com/22442407/care-for-caregivers-mental-health-covid.
Meadowmere and Mitchell Manor Oak Creek. (2023). Memory Care in Oak Creek, WI. Retrieved March 27, 2023, from https://www.fivestarseniorliving.com/communities/wi/oak-creek/meadowmere-mitchell-manor-oak-creek/memory-care.
NAC. (2020). Caregiving in the U.S. NAC. Retrieved March 27, 2023, from https://www.caregiving.org/research/caregiving-in-the-us/.
Ranji, U. et al. (2021). Women, Work, and Family During COVID-19: Findings from the KFF Women’s Health Survey. KFF. Retrieved March 27, 2023, from https://www.kff.org/womens-health-policy/issue-brief/women-work-and-family-during-covid-19-findings-from-the-kff-womens-health-survey/.
Rothschild, P. (2021). Supporting unpaid caregivers in crisis: A talk with Alexandra Drane. Mckinsey. Retrieved March 27, 2023, from https://www.mckinsey.com/industries/healthcare/our-insights/supporting-unpaid-caregivers-in-crisis-a-talk-with-alexandra-drane.
