America is the land of the free and home of the brave. It is the land of opportunity where so many have come to try to live their own American dream and make it big. However, this country is in no way perfect and has a handful of glaring flaws, one of the biggest and most significant being the healthcare system. Still, throughout the nation’s history, we have shown the ability to recognize our flaws, address them, and turn out better in the end. The healthcare system is broken, but not beyond repair. The key is finding exactly where and why it is broken and then repairing it piece by piece, brick by brick.

Trials and Failures
America is the world’s largest economy by nominal GDP and spends more on health care than any other country. Despite this fact, the US scores surprisingly poorly on a variety of key health measures, such as life expectancy, preventable hospitable admissions, suicide, maternal mortality, and obesity rate4. In this country, it is mostly pay to win, but many are still paying a lot just to continue to get the short end of the stick.
Certain efforts are geared towards improving the current system, but many of them do not address any of the root causes of these current issues. In fact, the majority of the investments in the healthcare system simply perpetuate and intensify the system’s flaws. For one, there is an extreme overemphasis on procedures and drugs4. While these options should generally be seen as secondary, tertiary, or last resort alternatives, they make up a sizable chunk of primary treatment decisions. These options can be helpful and beneficial, but they are often burdensome on the body and usually come with a collection of side effects making them less than ideal. Focusing on drugs and procedures has also led to a high emphasis on technology and specialty care4. Innovation in these fields can be very exciting and life changing for many people, but it also diminishes the attention towards promoting basic health practices such as nutrition, exercise, mental health, and primary care in general. This is extremely problematic as ignoring these components of people’s lives is often what leads to the more serious health issues.
Building From the Ground Up
Since there are so many problems that can be prevented, addressed, and treated on the primary care level, there needs to be more emphasis on its importance. Due to social media and pop culture, people often get lost in the alure and flare of the operating room, dramatic technological innovation, and breakthroughs in medical research. Shows like Grey’s Anatomy or ER demonstrate the adrenaline, excitement, and miraculous effects of surgery and medical innovation, and these values and perspectives seep into the viewers mind, distorting the image of the real healthcare system in its entirety. Each of these components holds intrinsic value but can overshadow the power and impact of incremental primary care2.
“Governments everywhere tend to drastically undervalue incrementalism and overvalue heroism.”
Atul Gawande from the New Yorker2
I have seen this firsthand when my own little sister’s life was saved because of the attention, care, and intuition of her primary care physician, Dr. Nicholas Kyriazi. My older sister, myself, and my younger brother all had the same doctor, so our family had a good, long-standing relationship with him. One day, during a routine check-up, he was listening to my little sister’s heart and noticed the rhythm was slightly off. He notified my mom that he had identified a heart arrythmia and advised that she follow up with a cardiologist to confirm and seek proper treatment. Through a variety of tests and scans, the cardiologist confirmed what Dr. Kyriazi had detected with his stethoscope. The cardiologist found a small hole in my sister’s heart which was the source of the arrythmia. However, since it had been caught so early on, there was plenty of time to address the issue and ensure the best treatment be put in place. At 5 years old, my little sister had successful open-heart surgery to repair the hole in her heart, and she is now a fully healthy and happy 15-year-old having no issues since. The surgeon directly resolved the issue in the end, but Dr. Kyriazi identified the problem and gave our family plenty of time to find the best solution. He is a hero.
Giving Care to Those Who Need It Most
“Until today, I didn’t know what a leaf looked like.”
4 year old child after receiving glasses for the first time at RAM3
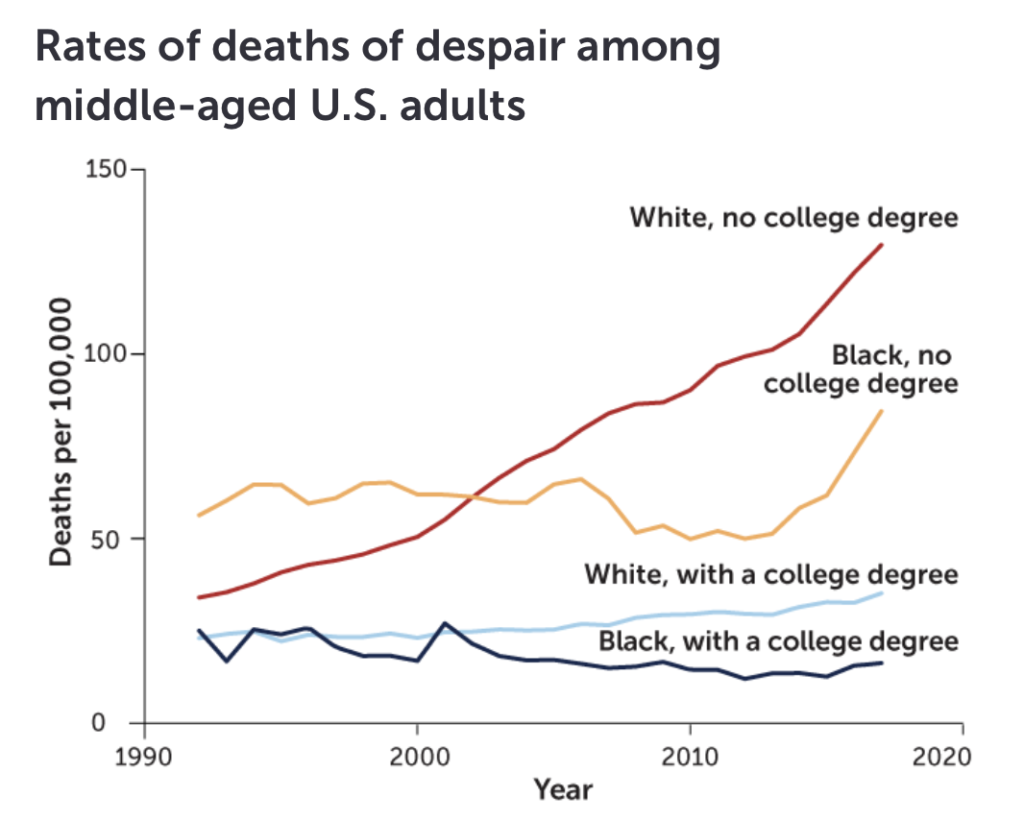
My sister needed a hero, and there are plenty more out there who need a hero just as much if not more than she did. A multitude of those in need are suffering from more than just medical issues. One of these groups includes middle-aged, non-Hispanic white people, especially those without a college degree. Throughout the past few decades, this group in particular has experienced a spike in mortality, identified by a Princeton University study1. These so-called “deaths of despair” include “white, working-class people ages 45 to 54 were drinking themselves to death with alcohol, accidentally overdosing on opioids and other drugs, and killing themselves, often by shooting or hanging1.” These source from four main indicators which include feelings of hopelessness, having low self-esteem, feeling unloved, and worrying frequently. Both the deaths and the associated indicators are evidence of the social determinants of health.
There have been efforts to address these issues and kickstart some reparations to this broken system. Organizations such as Remote Area Medical have made an incredible impact in these rural communities of Appalachia. They travel and set up large medical clinics in rural areas where they provide free medical, vision, and dental treatment to people who generally do not have financial or geographical access to healthcare3. They provide relatively simple care, but the effects of what they do change the lives of so many underserved individuals. Organizations like RAM and individuals like Dr. Kyriazi represent the small yet powerful solutions to our broken system. Recognize them, celebrate them, and emphasize their power and importance.
References
1Bower, Bruce. “’Deaths of Despair’ Are Rising. It’s Time to Define Despair.” Science News, 2 Nov. 2020, https://www.sciencenews.org/article/deaths-of-despair-depression-mental-health-covid-19-pandemic.
2Gawande, Atul. “The Heroism of Incremental Care.” The New Yorker, 16 Jan. 2017, https://www.newyorker.com/magazine/2017/01/23/the-heroism-of-incremental-care.
3Reichart, Jeff and Farihah Zaman, directors. Remote Area Medical. Candescent Films, 2013.
4Robert H. Shmerling, MD. “Is Our Healthcare System Broken?” Harvard Health, 13 July 2021, https://www.health.harvard.edu/blog/is-our-healthcare-system-broken-202107132542.
5Tikkanen, Roosa, and Melinda K Abrams. “U.S. Health Care from a Global Perspective, 2019: Higher Spending, Worse Outcomes?” U.S. Health Care from a Global Perspective, 2019 | Commonwealth Fund, 30 Jan. 2020, https://www.commonwealthfund.org/publications/issue-briefs/2020/jan/us-health-care-global-perspective-2019?gclid=Cj0KCQjw7pKFBhDUARIsAFUoMDbVZBN2PrzOlYBZvEe8qGs1PvCiAAxHemHZb_FjjCnAbSdQ0LSPChYaAmLYEALw_wcB.
