Michael Murakami
One fall in middle school I played for a Japanese baseball team. Although I speak little Japanese, a friend of mine recruited me when a teammate moved back to Tokyo. Practices and games mostly mirrored my other teams, except for conditioning. We worked the same routine at every practice which far exceeded a warm-up jog and stretching. I struggle to recall many of the exercises (granted, most names were in Japanese) except for two. The first began when our head coach yelled “Spi-der-man” in three, slow, drawn-out syllables. We repeatedly propped ourselves up with arms and legs extended outward and bodies held inches above the ground until we collapsed. The other consisted of shutter runs in the gym under time pressure until you either collapsed or quit. As the least fit member of the team, I felt embarrassed during conditioning since I always quit first. Even more confusing, at the end of each practice, we lined up and bowed, yelling “Arigato gozaimashita!” (thank you very much) to our coaches for leading the workout. Although perhaps atypical for youth sports, this experience illustrates a modern characteristic of exercise: we physically punish ourselves in the name of fitness out of a desire to avoid negative outcomes alongside pursuing positive outcomes…and then give thanks for the suffering. The old carrot that motivated exercise, the desire for health and wellness, recently became accompanied by a larger fear of the stick: stigmas and public shame.
The Carrot and the Stick1
Posited Virtues of Exercise
Exercise as an intentional activity (rather than indirectly resulting from manual labor) initially gained popularity for its positive physical and mental outcomes. Before analyzing the recent shift in mindset surrounding exercise, it is essential to acknowledge the benefits of and reinforce the need for a moderately strenuous exercise routine. First, exercise yields numerous positive physical outcomes. In his paper, Health Benefits of Exercise, Greg Ruegsegger explains how exercise is strongly correlated to an extended lifespan and the delayed onset of dozens of conditions and diseases, which improves peoples’ quality of life.2 Further, exercise benefits mental health. Kathleen Mikkelsen explains in Exercise and Mental Health how activity alters peoples’ moods positively and improves symptoms of anxiety, stress, and depression.3 Moreover, in the long term, exercise, especially endurance training, improves the overall mental health of those who partake.
On the one hand, this makes sense since better physical shape can make parts of life easier. Moving and performing enjoyable activities may reasonably increase one’s happiness. On the other hand, rather than being hedonically motivated, exercise may improve one’s quality of life and mental health by escaping from the negative societal implications of being viewed as “unhealthy.”
Modern culture rewards good health and, to people who fall into the “healthy” category, the positive attributes of exercise appear to be an achievable outcome. While this belief may seem reasonable and even beneficial in an isolated state (one may believe that these positive affirmations of exercise would encourage the healthy behavior of exercise), the implicit negative sentiments created about those determined to be in “poor” health are undeniably damaging. The following three sections will illustrate different sides of the same coin: negative stigmas surrounding poor health and positive reinforcement of dangerous “healthy” mindsets and activities.
Stigmas of a Lack of Exercise and Poor Health
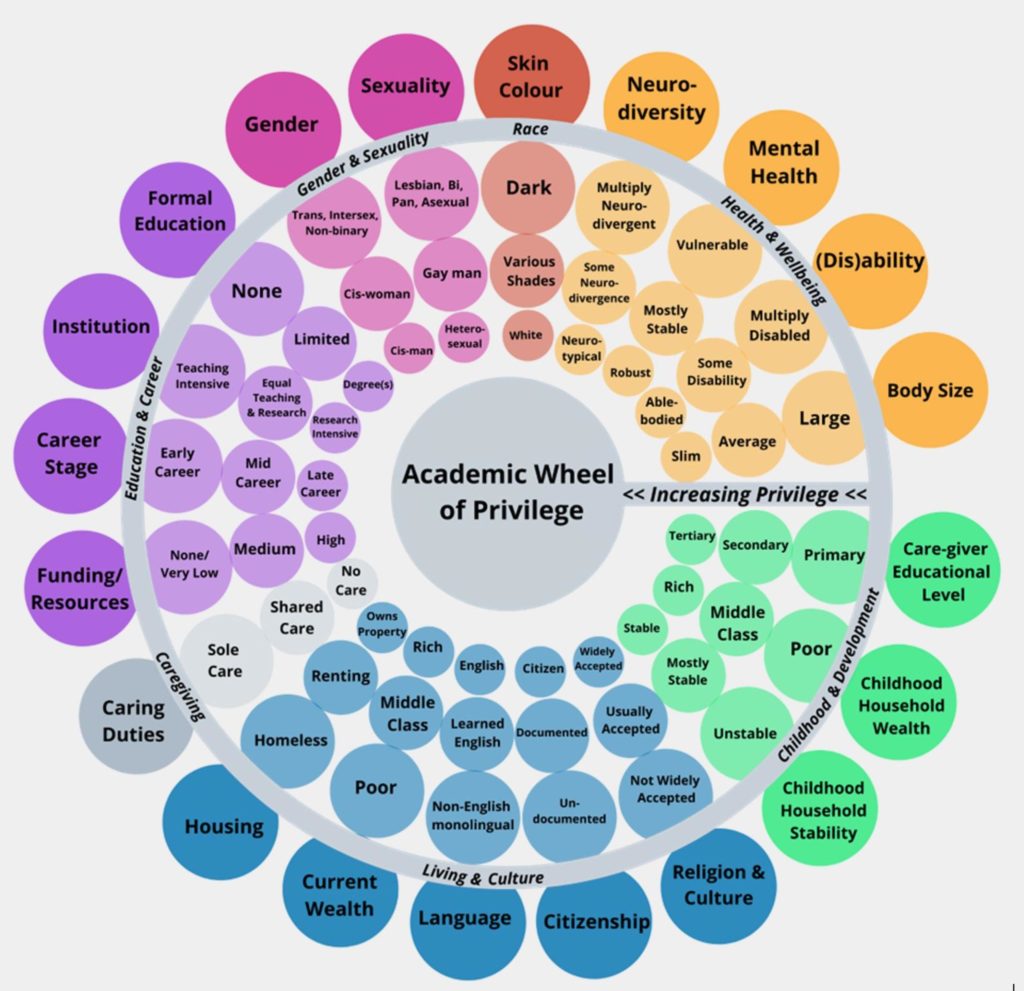
In chapter 10 of Illness Narratives, Arthur Kleinman describes how we derive the term “stigma” from Greek, referring to “marks that publicly disgraced the person.”4 Especially in ancient societies, many stigmas plagued societies’ social structure. Societies commonly developed stigmas about race, gender, wealth/social class, and a plethora of other visible characteristics. In modern society, as we attempt to reconcile historical inequalities equitably, new stigmas have arisen in the name of a seemingly “beneficial” characteristic: health. The primary issue is that stigmas surrounding health create a false sense of causation between the size/shape of the body (a physical attribute) and the overall health of a person (a generally non-physical characteristic). The result is that stigmas against those viewed as “unhealthy” only target people who appear to be overweight, which dangerously fails to capture reality.
To disprove that physical appearance and health are necessarily causally related, I will provide two examples. First, some people eat diets that are objectively unhealthy (per standard medical dietary standards) and/or perform health-damaging activities like smoking or vaping and appear healthy since their bodies have quicker metabolisms or the effects of their actions are long-term, not yet harming the individual. Since stigmas attack physical characteristics, they would not be stigmatized as “unhealthy” since (often) the consequences of their actions are not realized in the short-term.
The second example is the overuse of socially acceptable substances. The majority of US adults consume caffeine daily,5 and a large number drink or otherwise consume unhealthy amounts (greater than the recommended maximum of 400 mg per day). In fact, popular energy drinks like BANG and Reign contain nearly this much caffeine in each can. However, given that caffeine is a socially acceptable, productivity-boosting drug and it is difficult to measure another’s consumption throughout the day, certain substance abuse remains generally unstigmatized.
Since the results of these activities are not generally visible and/or are socially accepted, the seemingly only prevailing stigma attacks people labeled as “unhealthy” due to appearing overweight. Even worse, stigmas are not limited to adults. One notable campaign attacked children for their obesity in the early 2010s. Strong4Life created advertisements like the one below which demonizes fat children and asserts the need for lifestyle changes. It is truly unimaginable that any marketing department would consider this a promising advertisement, which could only happen after they approve it as acceptable. Neither feels right.

Medicalization of Exercise
Once understanding this stance taken on people viewed as “unhealthy,” it is next important to understand how society changed as a result. In Medicine as an Institution of Social Control, Irving Zola describes how medicine and “health” became an institution of social control. This shift results from medicalization, or the integration of medicine and medical research into everyday activities that otherwise would be separated.7 Play for children and exercise for adults recently became medicalized, from programs like Play 608 to the daily tracking of activities towards goals like counting steps, measuring the distance walked, and tracking heart rate on devices like Apple Watches. Many industries took this a step further, with employers pressuring employees to exercise by rewarding tracked activity monetarily (my firm, PwC, utilizes a program named VirginPulse9) and insurers creating programs called “interactive life policies”10 which personalize rates and create discounts based on continually tracked health metrics.
While some people enjoy optimizing their exercise and routines, this data collection represents a dangerous external motivation that destroys the equilibrium activity level for others. External motivation can result from third parties who directly benefit from someone becoming more “healthy,” such as an employer or insurer, or more innocently from friends. Apps such as Apple Fitness+, Strava, and Garmin Connect, all three of which I personally use, motivate activity through comparisons to friends and direct competition against others for more calories burned, miles run, etc. Since the data is public, even those considered “healthy” by society face new stigmas if they fail to hit their move goals on any given day. Such layered stigma and motivation perpetuate and exponentiate the toxic nature of the fitness industry by creating a desire for perfection in action and perfection in results.

Rotten Carrots: The Faux Acclaim of Physical Perfection
When someone pursues the health benefits of exercise to an extreme, the positive physical and mental health outcomes quickly disappear. A factor creating the culture of excess in exercise is blatant in fitness-related social media, specifically in the language influencers use. The industry is infested with lies and unreasonable extremism which pollute the mindset of a balanced person. First, social media highlights influencers who mislead audiences about their lifestyle, the use of performance-enhancing drugs (PEDs) to exponentiate their outcomes, and more. The average person is constantly exposed to unattainable physiques which may swing them in one of two directions: either their relative lack of progress compared to a PED user discourages them from continuing a fitness lifestyle or it creates a mindset to overtrain in pursuit of unrealistic outcomes.
The first outcome is damaging simply because it discourages the pursuit of a healthy and balanced lifestyle. Any of the aforementioned positive outcomes of fitness disappear and the person’s overall quality of life generally decreases. This is clearly undesirable.
The second outcome is potentially more dangerous. Although some of the physical benefits of exercise relative to a sedimentary life may still be realized at the highest level, many mental health benefits are quickly wiped away. This unfortunate outcome happens for a few reasons. First, as training becomes a larger part of someone’s day, other aspects of life must be minimized. The marginal benefit of additional exercise is mitigated by losing time for sleep, relationships, and other activities, all of which damage a person’s mental health. Further, the language found in the extremes of the fitness industry creates punishing mentalities that take mental and physical tolls on people. A clear example comes from David Goggins, former Navy SEAL turned fitness influencer who in his social media clips and books routinely encourages this mentality of excess and extremism with quotes like:
“We’re either getting better or we’re getting worse,”
David Goggins, Can’t Hurt Me
“Don’t stop when you’re tired. Stop when you’re done.”12
The Exercise Paradigm Shift: From Play to Work
Goggins and similar fitness influencers exemplify the overall paradigm shift found in exercise that Gabriel Winant describes succinctly; “Once associated with play, exercise is now closer to a form of labor: measured, timed, and financially incentivized by employers and insurers.”13 Here we find a dramatic shift. In our society fueled by a desire for progress and productivity, a growing proportion of our lives transform into new forms of labor. And much like other so-called jobs, forms of workaholism and gross excess appear. This flawed view of exercise that resulted from this shift quickly damaged society.
In the end, balance is important. There is no question that there are various benefits to physical activity that ought to be neither overlooked nor ignored, but taken to an extreme, the fruits of our labor quickly become rotten carrots that we endlessly continue to pursue. Although difficult in a productivity-focused world, it is imperative that our culture accept and normalize a moderate, healthy amount of exercise without slipping into unnecessary extremes or abandoning fitness altogether. In my opinion, this is most important for children. Rather than the rigid minds of adults who may already habitually follow an extreme, children should be shielded from exposure to an unhealthy form of labor. Such a shift would allow future children to not fear Sunday morning baseball practice as I did, but to look forward to time with friends playing a game they love. At a minimum, society ought to let kids be kids again by encouraging them to play in any condition, rain or shine, rather than mandate exercise and conditioning.

Works Cited
- Taylor, Justin, “Donkeys, Carrots, Sticks—and the Gospel.” The Gospel Coalition, 5 Dec. 2011, www.thegospelcoalition.org/blogs/justin-taylor/donkeys-carrots-sticks-and-the-gospel/.
- Ruegsegger, Gregory N., and Frank W. Booth. “Health benefits of exercise.” Cold Spring Harbor perspectives in medicine 8.7 (2018): a029694.
- Mikkelsen, Kathleen, et al. “Exercise and mental health.” Maturitas 106 (2017): 48-56.
- Kleinman, Arthur. Illness Narratives: Suffering, Healing, and the Human Condition. BASIC Books, 2020.
- “National Coffee Association.” NCA, www.ncausa.org/Newsroom/NCA-releases-Atlas-of-American-Coffee.
- Lohr, Kathy. “Controversy Swirls around Harsh Anti-Obesity Ads.” KERA News, 24 Aug. 2020, www.keranews.org/2012-01-09/controversy-swirls-around-harsh-anti-obesity-ads.
- Zola, Irving Kenneth. “Medicine as an Institution of Social Control.” Ekistics, vol. 41, no. 245, 1976, pp. 210–14. JSTOR, http://www.jstor.org/stable/43618673. Accessed 20 Mar. 2023.
- “Official Site of the National Football League.” NFL.com, www.nfl.com/causes/play60/.
- “Changing Lives for Good.” Virgin Pulse, 2 Dec. 2022, www.virginpulse.com/.
- Barlyn, Suzanne. “Strap on the Fitbit: John Hancock to Sell Only Interactive Life Insurance.” Reuters, Thomson Reuters, 19 Sept. 2018, www.reuters.com/article/us-manulife-financi-john-hancock-lifeins-idUSKCN1LZ1WL.
- “How to Start an Activity Competition with a Friend in Watchos 5.” MacRumors, www.macrumors.com/how-to/start-an-activity-competition-in-watches-5//.
- Goggins, David. Can’t Hurt Me: Master Your Mind and Defy the Odds. Lioncrest Publishing, 2020.
- Winant, Gabriel. “A Radical Critique of Wellness Culture.” The New Republic, 23 Mar. 2023, newrepublic.com/article/148296/barbara-Ehrenreich-radical-critique-wellness-culture.