On this episode of the Biomechanics in the Wild podcast, Ben James sits down with Dr. Raymond Klug, a board certified orthopedic surgeon practicing in Orange County, California, who specializes in complex shoulder and elbow reconstruction. They talked about his path into medicine and orthopedics and all things related to shoulder replacement, ending with a discussion about Dr. Klug’s own design work relating to shoulder replacement and where he would like to see the field of orthopedics go in the future.
- Introduction: start – 3:13
- What drew Dr. Klug to medicine and specifically orthopedics: 3:13 – 22:29
- Shoulder Replacement Discussion: 22:29 – 57:02
- Dr. Klug’s Shoulder Prosthesis Design Work: 57:02 – 1:06:16
- Where Dr. Klug hopes the field of orthopedics goes over the next 20 years: 1:06:16 – end
Ben James: Welcome everybody to the Biomechanics in the Wild podcast. Really happy to have Dr. Raymond Klug here today to talk with us about orthopedics and shoulder replacements. Dr. Klug, how are you doing today?
Dr. Raymond Klug: Good. How are you?
Ben James: I’m doing pretty well. Finals is approaching so I’m looking forward to the end of the year.
Dr. Klug: Oh, good. Congratulations. Are you done at the end of this year? Are you done at the end of the calendar year?
Ben James: No. I have one more semester after this one and then I will be done with my four years here. It’s going by really quick but looking forward to what the future has in store.
Dr. Klug: You only have six more months to prevent getting kicked out?
Ben James: Yes, hopefully. That is the goal. Hopefully, I can make my mom proud. I thought, why not doing that? Awesome. I know that we’ve worked a lot in the past before. I’ve been shadowing at Dr. Klug’s practice for the past two summers. If you want to just introduce yourself briefly, talk about what your specialty is.
Dr. Klug: I’m Ray Klug. I’m from Orange County, California. I grew up in an area called Cypress, which is a little town in Orange County. I went to Cypress High School, which is also where Ben went and which is how I know his mom. She was a patient of mine and mentioned that he was at Cypress High School. Then I went to Cypress College for a couple of years and then transferred to UC San Diego. I did undergraduate there and then I went to Chicago Medical School and did a master’s in physiology for a year. Then I did medical school, which is another four years. After that, I stayed in Chicago, went to University of Illinois, Chicago for residency in orthopedics.
Then I did a shoulder elbow reconstruction fellowship at Mount Sinai in New York. I went to a Mayo Clinic to be a visiting clinician in Rochester, Minnesota in complex elbow surgery. That was 2007. Then I went back again in 2017 to do basically scapular thoracic disorders, which are problems with the shoulder blade as it relates to the chest wall and how it affects problems with the shoulder.
Ben James: Awesome. It sounds like a lot of schooling. I guess how many years in total, I guess after high school does it take to become an orthopedic surgeon? You mentioned you did a few fellowships after that, but generally, how long does it take?
Dr. Klug: If you go straight through and you finish high school, say, at 18, undergrad, if you go through four years, then four years medical school, five years orthopedic residency.
Then if you want to be a subspecialist, then you do what’s called a fellowship, and most of the fellowships in orthopedics are an extra year. Some of them are two years, but most of them are one year. I don’t know what that ends up being. I can’t count that high.
Ben James: Too many years, yes. I guess firstly, what drew you to medicine in general? Then more specifically, how did you get into orthopedics?
Dr. Klug: When I was in high school, I was a reasonably competitive soccer player. Then when I went to college, I got hurt and basically never really played competitively again. Part of why I never played competitively again is because I had an orthopedic surgeon that didn’t pay attention to what I had and didn’t really listen, and was very quick to be in and out of there, and did surgery once, and I kept telling him there was a problem and he ignored me and back. That was 1990, I think 1990. At that time, there was no internet to find second opinions. There wasn’t a very good way of figuring out that if I don’t think this guy is telling me what I need to know, then I need to find somebody that really knows what they’re doing. At that time, it was the phone book and word of mouth. Basically, I got another opinion by one of his colleagues who said the same thing.
I missed my first year of college soccer because that’s when I got injured and had my first surgery. I tried to come back the next year and got re-injured at the first game basically. Then I sat out the second year. Then I transferred and didn’t bother trying out again because I was too busy doing other things. Then I had my second surgery, I think, yes, second surgery, and- third or fourth year of college, missed that year and then the next year. Then I eventually came out and tried out again as a fifth-year senior. By that time, I had two surgeries, hadn’t played in five years, and was just out of shape, et cetera. I have a little bit of a personal history of orthopedics as a patient, but aside from that, I was always just analytical and into science and mechanics and things like that. It made sense for me to go to medicine, and then within medicine, it made sense to do orthopedics.
Ben James: Awesome. Then you mentioned before, that you did some shoulder elbow fellowships afterwards. When did that come about and what point during residency or medical school did you think maybe shoulder elbow specifically within orthopedics?
Dr. Klug: During medical school, you have to figure out what your specialty is. My specialty is orthopedics. There’s internal medicine, family practice, general surgery, cardiology, neurology, radiology, et cetera. Typically, relatively quickly in medical school, you figure out you’re either a surgical person, a medical person, or an “other.” The other people are people that are either very scientific and don’t want to interact with patients, or they just want to do research, or they want to–
Radiology, for example, they just want to sit in front of a computer screen, or a pathology where basically, they just want to look at stuff under the microscope. Those specialties are relatively uncommon, although they are medical specialties. Basically, you figure out whether you’re a medical person or a surgical person, or neither one. What you find is the way they teach in medical school is, the first couple years, you do a bunch of stuff in the classroom. In general, medical school is four years.
First two years are classrooms, second two years is in the clinics. In the first two years, first year is for all practical purposes, normal body functions. That’s where they teach you normal stuff. Then in the second year is when they teach you all the abnormal stuff, pathology, infectious diseases, microbiology, pharmacology, all the stuff when things go wrong. Then third year is when you start doing your clinical rotations. There’s some required rotations, medicine, surgery, neurology, psychiatry, OB-GYN. I can’t remember all the rest of them. Then there’s some electives. Once you get to the clinical part of it, in third year, you find that there’s a way that they teach medicine aside from just handing a book and saying, “Here, read this, and the test will be in six weeks.” They have this thought process of ruling things in and out.
If somebody comes in with abdominal pain, for example, you do what’s called a differential diagnosis. Meaning you come up with a list of all the things that you think it could be, and then you figure out how you’re going to rule in or rule out each one of those things. Ruling in, ruling out means figuring out if it is this or it isn’t this. Essentially, what you do is you come up with a differential diagnosis and then you figure out how to rule out different things from that list. Then as you go through it, the list gets shorter and shorter and shorter, and assuming you started off with a proper list, then at the end, once you’ve ruled out all the things that it can’t be, then you figure out what it is. That is the traditional way of clinical medicine teaching.
What you find in medical school is there’s a lot of people that learn that thought process and they go through it, they really like it, and they thrive on it, et cetera, and those are the “medical people”, internal medicine, family practice, et cetera. The surgical people are a little bit different in that they want to– First, they want to physically fix things. They like working with their hands. They like figuring out if this thing’s broken or ruptured or whatever, I need to actually physically repair it by putting it back together, sewing it, et cetera, whatever, or excising it if something’s damaged so bad that it can’t be repaired.
The other thing is they generally don’t really like going through the whole differential diagnosis process. Obviously, I have a certain bias, but for the most part, if somebody comes to me in my office with shoulder pain, I can usually tell them what it is without even knowing what their– When did it happen, how did it happen, all the questions, et cetera, within– I can tell them it’s one of these three or four things, and then I just do the exams or the x-rays, exam meaning the physical exam, making them do this and do this and put your arm this way and that way and figure out what hurts and what doesn’t hurt.
In order to figure out what they have without going through a formal list of– there’s 27 things that this could be, because I already know it’s not the first 24 of them. You could argue in a way we’re doing the same thing, differential diagnosis and rule-outs, but we– The surgical people are a little bit more of the mindset that we’re going to skip a lot of those steps and just cut to the chase. The way I explain it, I understand it might sound like your response will be, “Well, obviously that’s what you want to do”, but maybe the reason why you think that is because I explained it from a certain bias point of view because that’s the way I think about it.
Anyways, so relatively quickly in medical school, you figure out you’re either a surgical person, a medical person, or an other. Then once you do that, then you just have to figure out what specialty you’re doing. Once you figure out you’re a surgical person, you just have to figure out what specialty it is. Aside from my personal history as an orthopedic patient, when I was a kid– When I was young, I don’t know, I used to race BMX bikes and I was a competitive skateboarder and I used to take apart bikes and build things, et cetera. When I went to high school, I worked on car stereos, I did installations and that stuff.
I rebuilt interiors, et cetera. Around the time I finished high school, I had old classic cars I used to work on, I rebuilt motors, et cetera. To me, I always liked working with my hands, which is surgery. I also liked tools and power tools, which is mostly suited towards orthopedics. Some of it is just simply picking how bigger things you want to work on versus how small. If you do eye surgery, you’re working on very small things and another thing you have to look at is how sick do you want your patients to be. The nice thing about orthopedics is the patients are generally healthy because they’re usually young and they’re generally happy with the outcome of what we do for them. We usually make them better and they stay better and then they get back to how their life was.
Whereas a lot of other fields in medicine, internal medicine for example, they basically take somebody that is chronically ill and as they’re going downhill, they tune them up and then they go downhill a little bit more, then they tune them up and they go downhill little bit more and then they gradually go further and further downhill and then you can’t really fix a lot of the stuff. You could argue that perhaps it’s that people in orthopedics have a short attention span. We want things fixed and done so we don’t have to spend too much time on it. I guess it’s a difference of personalities. You have to think about how sick you want your patients to be. If you’re a neurosurgeon, you might end up with a third of your patients dying.
In ortho, I almost never have a patient die. I don’t remember when’s the last time I had a patient die. I don’t like calling families and telling them bad news and things like that and I don’t like being in that situation. I also like the ability to say, “Well, this is elective surgery. If you need a knee replacement and for example, if you have a bad heart or bad lungs or you’re too high risk for anesthesia, we can just choose to not do it.” Whereas if you’re a cancer surgeon or a neurosurgeon for example, or cardiac surgeon, cardiac surgery for example, if somebody’s got a bad heart, you have to operate on them even though you know there’s a 20% chance they’re not going to survive surgery. If you start thinking about if there’s a 20% chance this person’s not going to survive surgery, that means 1 out of every 5 patients that has this is going to die. Like I said, I don’t like having patients die. [laughs] I don’t like having to tell families that their family member didn’t make it.
Ben James: Definitely. I imagine that could be really tough. I guess I’m glad to hear that that doesn’t happen all the time in orthopedics. I guess did that happen more frequently in residency or at the beginning part of your training or it’s pretty consistent throughout your time in practice?
Dr. Klug: Well, there is certain subspecialties of orthopedics where patients are more likely to die. Complex spine surgery where they have these huge surgeries, there’s a much higher mortality rate and complex joint replacements because typically if somebody comes in that’s 65 and healthy and has a knee replacement, everything’s fine and then it wears out 20 or 30 years later. By that time, they got bad bone quality. They’re now 85 or 90 years-old, they have a bunch of other medical issues and the surgery is a much bigger surgery, much more blood loss, much more high risk.
There’s a decent chance it could be infected, which means they’re going to get six or eight weeks of IV antibiotics, they’re going to be bedbound for that time, which has a whole host of other complications. In shoulder and elbow surgery, it’s very uncommon because one of the big things that predisposes people to poor outcomes is immobility, being bedbound no matter how bad your shoulder or elbow is, you’re never really bedbound. When I was in residency and we did all the different specialties, joints and spine and hand and a bunch of other stuff, pediatrics and trauma, et cetera, then the joints guys would have patients that died once in a while and the spine guy would have patients that died once in a while.
The shoulder guy and the sports guy and the hand guy, they never had patients that died. The peds people almost never had patients that died either. That’s a whole different story if you’re interested in pediatrics. In the beginning, in residency I was– In residency, you’re essentially like an apprentice to somebody else. You’re assisting with their patients. If the guy you’re assisting is doing a lot of complex joint replacements and there’re big high-risk surgeries, then you’re going to see patients dying and you’re going to have to deal with families of patients that died. They’re not technically my patients. Ever since I’ve been in practice, I’ve never really had very many people die. I don’t know, I don’t think- I’ve never had somebody die on the table.
I’ve had a few times where somebody coded on the table, canceled surgery, resuscitated them, and then they died the next day or over the weekend or something like that. Thankfully, the three or five times that that’s happened in 15 years, it’s never been the result of my surgery. It’s that they have something that needs surgery and I can’t really avoid it and they’re just so sick that this is a risk that they have to take.
Ben James: You mentioned before that a lot of the time it’s elective surgery. I guess what percentage of the surgeries that you do is more of the elective, do it when they’re able to do it versus something that’s an emergent situation where you have to go in and do it right away?
Dr. Klug: By far the majority is elective. I have an elective practice and then I’m chairman of the department of the hospital and we have an ER call panel and I’m on the call panel, which is voluntary. I just do it because the hospital I work primarily at is not a level-one trauma center, so we don’t really see a whole lot of very bad injuries. It’s mostly little old ladies with broken hips, where we are there’s– As you know, but I don’t know how the audience knows, this area of southern California, it’s got great weather and it’s got very healthy old people. When I was in medical school residency in Chicago and New York also, and Minnesota, I came back here in practice. I couldn’t believe how few people smoked out here. Practically nobody smokes out here.
Whereas when I was in those other places, it was every third or fourth patient I would have to give the smoking cessation lecture to. It was so rare that the patient smoked out here that I remember after a couple years of practice, I would walk in the room once every couple years and I’d go, “Smells like smoke in here. Do you smoke?”, because it was so unlikely that patients smoked. Now they got vaping and other stuff like that. Even with that, it’s still pretty uncommon that you would run into that and that was one of the big things that dictated poor outcomes.
Ben James: What about the smoking specifically was bad for type of surgery that you were doing?
Dr. Klug: Well, nicotine’s a vasoconstrictor, so it cuts down blood supplies, so it leads to wound healing problems, fracture healing problems, anytime you’re repairing tissue, you’re relying on the body. Basically when we repair anything, whether it’s a tendon or a bone or whatever, all we’re doing is putting the pieces back together and holding it in place while we’re waiting for the body to heal itself. In order for the body to heal itself, that tissue has to have a blood supply and basically, the body has to be able to increase blood flow to that area to get growth factors and proteins and hormones and all these healing, what do you call it? Cytokines and all this other stuff to the area. If you give them something that’s a vasoconstrictor that’s going to significantly limit blood flow to that area, not only are you limiting their ability to heal the injury that you’re trying to repair, but you’re also limiting the ability for them to heal the incision, the wound.
There’s much higher risk of wound infections or wound complications, and if a wound doesn’t heal, then eventually it gets infected, then if you got an infection then it can screw up the whole thing. Then also just the thing that you repaired, there’s an age-old saying that orthopedic hardware meaning plate, screws, rods, whatever we put in there, is always temporary fixation until the body heals the thing that you’re repairing. If the body doesn’t heal that, the hardware will eventually fail because it’s just every like every rod, every screw, every plate, or whatever, if you start bending it even microscopically back and forth a million times, eventually it’ll fail. The analogy we usually give people is if you take a paperclip and you bend it back and forth multiple times it will eventually break.
That’s the same thing that happens with rods and screws and everything else. If the thing is designed to be temporary fixation, and the body doesn’t heal it, eventually the hardware will break. Anyways, back to what I was getting at was out here very few people smoke, and we have great weather year-round, so we got all these 80 and 90-year-old people that are athletic, and swimming, and running. I have patients that were in their 80s and 90s doing this, I can’t remember what they call it but that’s like the masters track and field which for people over 65 or 70.
Ben James: Interesting.
Dr. Klug: Yes, it’s crazy. I tried telling them to stop doing the high jump, they do this stuff and I’m afraid they’re going to break their neck or something. Anyways, it’s nice being in an area where we have a population that’s very healthy. It ends up being good and bad because you end up with a lot of people that are able to have surgery at a much more elevated age because their health is so good. There’s only so much you can fix by being in good shape and diet and exercise and that sort of stuff. Their bone quality is still bad, their ability to heal wounds is still not so good, et cetera.
Ben James: Yes, and so the past couple summers I’ve been there a lot of what I’ve seen you do especially as a shoulder/elbow person is shoulder replacement, which I want to get into now. I guess shoulder replacement, it’s a big thing not only for you, but I guess it’s becoming more popular amongst the general population maybe over what, would you say the last 30 to 40 years or?
Dr. Klug: Probably 20 or so.
Ben James: Okay.
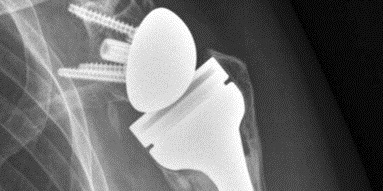
Dr. Klug: Shoulder replacements are the third most common major joint replacement after knee and hips. It’s becoming much more popular. Basically, in 2004, the reverse shoulder replacement was FDA approved in the states, and that really revolutionized how we treat bad shoulder problems that prior to that really had no real good treatment other than hope that it works okay. I have a certain perspective on medical treatment in general. Which is if you read articles and textbooks et cetera, et cetera, whatever condition you have, orthopedics for example, they’re going to list a bunch of different treatments but they never really give you a very good idea of how well these things work and how long they last. Whether you got whatever, bursitis, or tendonitis, or rotator cuff tear, or whatever, the textbook’s going to list all the same treatments.
Anti-inflammatories, pain medications, heat and ice, what do you call- activity modifications et cetera, and bracing, surgery, all the different surgeries et cetera, et cetera, et cetera. They don’t really give you a very good idea of which one of these works very well and which one doesn’t work very well. What ends up happening is you get all these general treatments for, treatments for everything. If you look at somebody that has a very bad rotator cuff tear that is so bad it can’t be repaired, if you look at the textbook, it will tell you the treatment for that is hemiarthroplasty which is partial shoulder replacement, but they don’t really make it very clear that it doesn’t work very well. It’s okay for pain control and if you have that condition you probably can’t lift your arm overhead, and doing that surgery doesn’t regain you the ability to lift your arm overhead. It can dislocate it’s got all these other issues et cetera, but that’s kind of what the treatment was for a bad rotator cuff tear prior to 2004 in the United States.
When we got the reverse shoulder replacement then, that really revolutionized the way we treated this and the reverse shoulder replacement. It’s made the treatment of these very bad conditions of the shoulder, so routine and the results were so good that we used to think of that as a salvage procedure and we call something a salvage procedure, that means that you don’t really have a good option so this is the best we can do because we can’t really think of anything that’s going to actually work, we’re just got to think of something. The reverse shoulder replacement used to be considered a salvage procedure, but I would argue that now the results of it are so good that I don’t know anybody that really thinks of it as a salvage procedure anymore.
It’s now considered like a first-line treatment because the results are so good. An anatomic shoulder replacement– The shoulder is basically a ball in socket. The ball is the top of the humerus, which is the upper arm bone and the top of it’s called the humeral head. The socket is the scapula. The glenoid process of the scapula. The glenoid is the socket of the shoulder blade. We used to do anatomic shoulder. We still do anatomic shoulder replacements meaning you replace, if the ball wears out you replace the ball with a new ball, and if the socket wears out you shave off the socket and put a cap on there to recreate the socket. Meaning you are restoring the normal anatomy, you’re replacing the ball with a ball and replacing the socket with the socket. What the reverse does is it flips the two. It puts the ball where the socket used to be and the socket where the ball used to be.
It gets a little complex on how it works, but basically, there’s several layers of muscle and tissue that have to work in concert with each other in order to allow the musculature of the shoulder to move the arm in space. The rotator cuff basically keeps the ball centered in the socket to make a long story short. If the rotator cuff doesn’t work, then the ball doesn’t stay centered in the socket. When it does that it basically creates a fulcrum. In order to lift your arm up basically what happens is the deltoid which attaches in the acromion which is right above the humerus, and then it inserts on the humerus.
Muscles only do one thing, they pull stuff and then they relax. They can’t push anything, if you need to, so if you want to bend your elbow for example, what you do is you fire your biceps and it pulls your forearm up. If you want to bring your forearm back down, you don’t necessarily have to fire your triceps to bring your elbow down, you just allow gravity to do it. What you do is you just stop firing your biceps and then gravity straightens your elbow. The biceps doesn’t actively straighten your elbow, and neither does the triceps unless you’re upside down.
Basically muscle for example the biceps only does one thing. It pulls and then it stops pulling, and then something else causes it to go the other direction, whether it’s gravity or a counterforce. I can’t remember what they call it but a muscle doing the opposite thing. In the shoulder, what happens is the deltoid is the primary mover of the shoulder, but in order for that to happen, the rotator cuff has to keep the ball centered in the socket to create a fulcrum. It’s kind of like a ball in socket joint. If the rotator cuff isn’t creating the fulcrum, then what happens is instead of the deltoid pulling the shoulder of the humerus up as a hinge it basically translates the shoulder the humerus up in line with the humerus.
Ben James: Then there’s no rotation in that case.
Dr. Klug: Yes, so then you lose, there’s no rotation, there’s no fulcrum so it basically, this is what I was talking about earlier. If you have a diagram, instead of lifting your arm like this what happens is if you fire your deltoid and you don’t have the fulcrum when you try to do this, what ends up happening is you do this.
Ben James: You just raise your shoulder up.
Dr. Klug: Your humerus just goes straight up in line with the humerus instead of rotating around to the shoulder joint. What the reverse shoulder replacement did by flipping the ball in the socket essentially what happened is it put the socket underneath the ball, and then by that happening that created the new fulcrum to allow the deltoid to lift the arm. In these people that have this condition, we call it rotator cuff tear arthropathy meaning somebody had a rotator cuff tear that is so bad that it’s irreparable. Since the ball is not staying centered in the socket anymore, the ball is causing uneven wear in the socket and then you develop arthropathy or arthritis of the joint by wearing out the cartilage and then it creates pain. Now with the reverse shoulder replacement, we have fantastic treatments for this.
I remember several times early on when I saw somebody that had done their first reverse shoulder replacement, they were incredulous. They couldn’t believe how good these things worked compared to what we were used to seeing. We used to tell people they, after a partial shoulder replacement, which is what you did for this before the reverse came out, that you should expect to get almost 90 degrees of elevation. 90 degrees of elevation means your humerus is parallel with the ground. With the reverse, you always get overhead. There’s a few times it doesn’t work, right? For all practical purposes, it’s like 95% of the patient get overhead activity. Again, you can get to the top of your head, you can do your hair in the back, you can get plates off the top shelf, you can climb a ladder.
I got patients playing golf and tennis and swimming and all that other stuff. That’s the big change that’s happened in shoulder surgery and especially shoulder replacements in the last 20 years and because of that, whereas it used to be just specialists like me did shoulder replacements. Now these things are, they’re doing so well that just general orthopedists and community surgeons are doing them. That’s really why shoulder replacements are getting so much more popular now. They used to say there’s about 400,000 hip replacements per year, 400,000 knee replacement per year, and about 40,000 shoulder replacements per year. Shoulder replacements are now up to almost a 100,000 a year. It’s more than doubled in the last 10, 15 years.
It’s not because people are getting better at doing the surgery, it’s because people are figuring out that the surgery works so well that they’re not afraid to try it. That’s another thing. I guess I should mention that traditionally people were afraid to do shoulder replacements because one, they’re not very experienced in it. Two, they didn’t have any training in it. Three, the outcomes are bad and people, surgeons don’t like having bad outcomes when potentially someone else could have gotten a better outcome. People don’t like being blamed for something not working, what– If you do something that never works, then nobody seems to complain about it, but if you do something that some guys do well and yours doesn’t work, then they look at you like there’s something wrong.
Ben James: What percentage of your patients, I guess now, would you say gets the normal anatomical shoulder replacement versus the reverse?
Dr. Klug: Mine is probably 90% reverse or maybe even more than that because what I said earlier is oversimplified of course. There’s a lot more to when you can do a reverse versus when you do an anatomic and especially me where I live, we have so many older people that have so many other things going on with their shoulders.
For all practical purposes, the way I think of an anatomic shoulder replacement is that an anatomic shoulder replacement works very well for somebody that only has arthritis to the shoulder with cartilage loss and nothing else going on. The rotator cuff’s fine, the bone is fine. That’s not too much bone loss. There’s not instability, there’s not all these other problems that can happen with the shoulder.
As you get older and people with multiple surgeries and previous surgeries, what you find is less and less people are the perfect candidate for an anatomic. Basically, the reverse fixes all those other things too. If somebody is a good candidate for anatomics, I do them, I did one last week, I did one a couple weeks ago, et cetera. I do a lot more reverses because if you really understand all the ways anatomics fail and the way the reverse makes up for a lot of this stuff, or you could say prophylactically treats some of this stuff because in the– The design allows, it allows you to treat things that you don’t know are a problem yet that may pop up five years from now or so.
Whereas if someone had an anatomic, you would have to convert it to a reverse. If you do a reverse in the first place and they have the same problem, then you don’t have to fix it anymore because it’s already fixed.
Ben James: Exactly. Then you get one surgery instead of two and if the patient’s older, it’s definitely better for them.
Dr. Klug: Exactly. The older they get, the higher risk they are for complications. Most of the complications I talk about are not orthopedic complications. They’re heart attack, stroke, blood clots, pneumonia, things like that. All the things associated with a unhealthy patient getting anesthesia. It’s very uncommon that they actually have an orthopedic complication with a shoulder replacement.
Ben James: Got it. I guess for, perhaps we can just talk about the reverse in terms of how the actual surgery happens. You want to talk a little bit about that? Actually going in, removing what you might remove for that specific surgery, and then putting in the joint?
Dr. Klug: Yes, basically there’s a few different approaches. When we talk about surgical approaches that tells you where you make the incision and what you go through or around in order to get to where you got to get to. When you go through surgical training, you have to learn all the surgical approaches. Basically, the principle is, for example, if you go through a muscle, that muscle is powered by a nerve and if you hit that nerve or cut it, then you will lose the function of that muscle. What you do is you have to either know where the nerves are, or you go through what we call inner nervous planes, whereas the muscle on the right side of something is innervated by one nerve and the muscle on the left side is innervated by a different nerve. You go between those two muscles so you’re not at risk of damaging a nerve crossing your surgical field.
Ben James: Got it.
Dr. Klug: We call them inner nervous planes. For the shoulder, the most common way to do a shoulder replacement is an anterior incision in the front. Basically, it goes from about the clavicle down to basically what we call the deltoid tuberosity, which is where the deloid inserts, but it’s essentially 45 inches diagonally across the front of the shoulder.
Ben James: Right.
Dr. Klug: That incision overlies the interval between the deltoid and the pectoralis major. Right between the deltoid and the pectoralis major is the cephalic vein. Basically, that’s the inner nervous plane. The peck major has two separate nerves, the petrol nerves that supply it, and the deltoid has the axillary nerve that supplies it. As you can imagine, just makes sense that if you’re at the end of the muscle, so the peck is medial to the deltoid, if you’re talking about the peck and you’re at the lateral border of the peck, then the nerve is not going to come in from lateral because the muscle is medial and you are already at the end of it.
The same thing is true with the deltoid. The deltoid is on the lateral side. If you go to the medial border of the deltoid, the nerve is not going to be coming in from medial to lateral.
It comes in from lateral to medial because you have gone to the end of the muscle. Basically, that’s the inner nervous plane, delta petrol interval. You go between the delta and the peck. You get the cephalic vein out of the way, you can bring it medial or lateral, whichever basically dealer’s choice. Then you go down and then the next layer you get to is essentially the fascia. It’s called the clavipectoral fascia. You open that and then underneath that you get to the humerus and the front and you get to the rotator cuff. In the rotator cuff, the one in the front is called the subscapularis. Then the supraspinatus is on top and infraspinatus and teres minor in the back.
You usually don’t really see those. What you have to do is you got to get into the joint by going through the subscapularis, usually. There are techniques of sparing the subscap, et cetera. That gets a little more esoteric and complex. Basically, you have to either cut the subscap tendon or you have to peel the subscap tendon off of the bone because muscle inserts on tendon, muscle inserts into tendon, tendon inserts on bone. That’s how you move stuff. You fire the muscle, the muscle pulls on the tendon, the tendon pulls on the bone. That part of the bone’s called the lesser tuberosity. The subscap inserts on the lesser tuberosity, you can either cut it off, you can peel it off, or you can osteotomize the lesser tuberosity in this plane, coronal plane, which is like up and down and cut a piece of bone with the muscle tendon unit off with it.
The reason why we do one versus the other is because every few years a new study comes out and says one way heals better than the other way. Once you do that and you take the subscap off the front, then you’re looking at the shoulder joint. You have to do that and then you have to, the capsule encloses the joint. It’s like, if you think about like a CV joint in a car, there’s a CV boot that goes around it. The CV boot basically encloses the joint and keeps the lube in there, so the capsule in the shoulder joint or in any articular joint essentially encloses the joint and keeps the fluid in there. The lube in this case is called synovial fluid, which is basically the lubricating fluid for the joint. The subscap is attached to the capsule.
Once you take the subscap off, the capsule comes with it. In my opinion, if you’re going to do a proper shoulder replacement, then you got to take out the capsule also. The reason for that is because the capsule tends to be contracted and tight, and if you don’t take it out, then– By taking it out, you can improve range of motion afterwards.
Once you do that, then you’re basically looking at the joint and then you dislocate the shoulder. If you’re doing it in what we call the beach chair position, the patient is sitting like they’re kind of in a lounge chair, then basically you do that just by rotating the arm out and then the shoulder pops out. Then you’re looking at the humerus. You basically take a cutting guide usually.
There’s some systems that just have a free-hand cut. There’s a cutting guide that you can put on the humerus or you can drill a hole on the top of the humerus, put a reamer down, which is basically like a giant drill bit, and then you clamp the cutting guide onto that, that drops down and tells you to make the cut in the correct height and rotation. Then you make the humeral cut.
Usually, once you do that, you prepare the humerus, which basically means you put bigger and bigger reamers in there until you figure out what size it is. The humerus is essentially a – You already made a hole at the top, so you put a long 6-millimeter drill bit down, then you put a 7-millimeter drill bit down, then you put an 8-millimeter and keep going until basically it starts to get tight.
Then the shoulder replacement looks like basically a tube with a thing sticking out of the side. You basically have a thing called a broach, which is shaped like the shoulder replacement and same thing, you put down a 6, you put down a 7, you put down an 8, and then you go, “Okay, it looks like it’s about a size 8.” Then you’ve prepared the humerus. Usually, you leave that broach or inserter or trial component or whatever in there just to protect the humerus while you go to the glenoid and prepare that, because basically there’s not a lot of space and you have retractors. They’re essentially like pry bars that allow you to pry the humerus out of the way so you can get to the glenoid to prepare the glenoid.
Around the glenoid is the labrum, which is basically– The shoulder is a ball and socket, the glenoid is the socket. The labrum is basically an O-ring around the socket. Basically, you take that out, and the capsule attaches to that. Usually, you’ve either already taken out the capsule or you take out the rest of the capsule. How much capsule you take out depends on how their motion is and how unstable they are, et cetera. Then you prepare the glenoid.
How you prepare the glenoid is different on different systems, but usually what you do is you find the center of it just by eyeballing it and you drill a hole in the middle of it, and then you have a reamer, which is a different type of reamer in this, which is more like a– A reamer for a hip is like a giant drill bit with a semi-circular cheese grater on the end of it. If you start with that, then you realize a shoulder is a socket just like a hip, but the socket is much more shallow. It kind of looks like that, but it’s just a curved thing, but there’s very little curvature to it because the socket in the shoulder is not very deep.
Then you figure out what size it is. They come in different sizes. Most of them just call it small, medium, or large, and you say, “Okay, I need a medium.” Usually, you put the small reamer down and then you clear off the excess cartilage and get down to good bleeding bone and then you put the medium reamer down and then you say, “Okay, that’s the size.”
For an anatomic shoulder replacement, the glenoid components are held in place by cement, so you drill some holes, there’s a jig that tells you– After you’ve drilled your center hole, which is what you use to put the reamer in, there’s a guide that sits in that hole and then that has a drill guide to put the other three holes. Most systems are three holes. Then you drill the other holes. You take everything out. If you’re me, you wash it out, you put in thrombin and peroxide and any other antibacterial stuff you can think of.
Then the glenoid component is a piece of plastic with pegs in it. Those pegs go into the holes you just created. Usually, we cement them in place. Cement is basically like grout. You take this powdered stuff on the back table and put a catalyst or polymer or whatever on it and then you mix it up and somebody watches the clock and they say, “Okay, it’s been one minute, so now you can put the cement in, and now it’s been eight minutes, so the cement should be dry,” et cetera.
The cement is kind of like play dough. Once you put the cement in, it starts gushing out the sides, then you got to scrape it out, then you sit there and wait for 10 or 15 minutes for the cement to dry. That’s usually when I ask everybody if they’ve got any jokes.
Ben James: They usually don’t, yes.
Dr. Klug: They never do. I think it’s also partially because I ask them the same thing every week, so if they had jokes last week, they won’t have them this week. Anyways, and then basically the glenoid is done, and then you go back to the humerus. Essentially, the head that you cut off before, their sizers that come in the kits, that tell you approximately what size it is. There’s other ways you can measure it, on the x-ray, or measure it on a CAT scan ahead of time, et cetera, and then you basically put the head, which is a ball. It’s kind of like a third of a circle. It’s less than a hemisphere, but basically, you put the ball on the stem that you already put in there.
Usually, it doesn’t sit right in the center of it, so they have these little offset things to figure out whether it’s going to be maximally offset at four o’clock on the clock face versus two o’clock on the clock face. Then different companies make different ones. One company makes a 1.5 millimeter, a 4.5 millimeter, another one that makes a 3 millimeter, et cetera.
Nowadays, we do all this stuff with CT, planning ahead of time. You take all these measurements ahead of time, you know what size you’re going to put in, et cetera. I do it with a GPS guidance system, which is a navigation system where we put a couple of pins in the scapula and then we have this little probe with a detector on it and then we paint the surfaces of the bone.
We’ve previously gotten a CAT scan of the patient, imported the CAT scan into the computer so then the computer knows where we are based on those points from where the probe is. Then there’s another one of those detectors on the drill shaft, the reamer shaft, the inserter shaft, et cetera. While you’re doing the reaming, it’ll tell you you’re at this angle and this depth and this inclination, et cetera, and the same thing with when you’re drilling the holes, et cetera. That’s just a newer technological advance.
Most of the time on the humeral side, you don’t use cement just because humeral fixation works fine without cement most of the time. If somebody has bad bone quality or it’s between sizes or something like that and doesn’t fix, then we just cement it. Cementing on the humeral side is the same thing. You mix up your play dough on the back table and you squirt it through a turkey baster and wait till it’s mostly dry and then you shove it in and then scoop the stuff out of the way that’s excess and then you ask if anybody knows any jokes.
Ben James: Most of the time it’s just press fit in there, though. Right?
Dr. Klug: On the humeral side, it’s usually press fit. There are systems that are designed to be cemented, but the thing about cement is cement doesn’t work any better statistically than non-cemented, and it takes an extra 15 minutes, maybe 20 minutes. If the whole surgery only takes an hour and 15 minutes, people don’t want to be sitting there for 20 minutes waiting for the cement to dry.
Then, once you get done with that, there’s– We call them trials. Anytime you have a trial, basically what it is, it’s a model of the prosthesis that comes in different sizes. Say for example, if you think you’re going to put in a size 9 stem, you put in a trial 9 stem to make sure it’s the right size. Then you trial the head on that. Then you trial the offset, trial the inclination, meaning the angle in this plane versus this plane, and trial the rotation, et cetera. Once you figure out where you want it, then you build the real prosthesis based on those parameters.
Depending on the system, you can either build it in the patient or you can build it on the back table and then put it in the patient, or you can do hybrids of both. Then, once you’ve done that, then essentially all that you do is look around, make sure nothing is bleeding, make sure you didn’t miss anything.
There’s a few other minor things you do, release adhesions to help range of motion. I always check the axillary nerve because it’s right in the surgical field, and if you have an axillary nerve problem, that’s a big problem in a shoulder replacement because that supplies the deltoid, and the deltoid is what this whole thing relies on to work. Then essentially you repair the subscapularis and then you close the wound.
Ben James: You said overall it usually takes around an hour and 15 minutes for the entire surgery?
Dr. Klug: Yes, somewhere around there. It depends. Reverses are faster because, on the reverse, the reverse is designed to function in people that don’t have a subscap, so many people don’t repair the subscap in reverses, and they seem to work fine. I go case by case depending on how bad it is and how their motion is with it and how tight it is, et cetera. The other thing is, in an anatomic shoulder replacement, you cement the glenoid.
On a reverse, you don’t cement either, so you’re saving 20 minutes by not cementing the humerus, 20 minutes by not cementing the glenoid, so reverse is actually usually faster because the subscap repair in an anatomic is– One of the reasons for failure of anatomics is failure of the subscapularis, as a lot of people put a lot of time and effort to doing a very good repair of the subscap, so that takes a lot more time too.
If I’m doing a reverse and the patient is thin, their blood pressure is down, they’re healthy, they’re not really struggling for exposure or anything like that, I’m usually about done in probably about 45 minutes, then I have an assistant that closes the wound. Usually, the OR starts at 7:30, the 7:30 case usually starts around 8:00, and I’m usually gone around 9:00, and then the surgical assistant closes the wound. Then I go and do paperwork in the computer and call the family and that sort of stuff. In an anatomic, it probably takes another half an hour. If you think about it, adding a half an hour to a case that only takes an hour is kind of a lot.
Ben James: Yes. I know in the past we talked about hip replacement specifically. There’s the osseointegration where the bone basically develops into the prosthesis. Is that similar in shoulder replacements?
Dr. Klug: Yes.
Ben James: Okay, so over time, that bone will grow into the replacement and make it stronger?
Dr. Klug: Yes. There’s different types of implant design. Some of them are ongrowth and some of them are ingrowth. The thing about the humerus, the nice thing about the humerus is– In the femur, for a hip replacement, you have the whole body weight going on it every time you step. In the shoulder, there’s not a whole lot of force that goes across it. We used to have ongrowth prostheses and ingrowth prostheses in the hip, but most of them are ingrowth nowadays because it’s stronger.
In the shoulder, since not only are the forces that go across it much less so you don’t need as good a fixation. Also, if the thing is infected or a problem, you got to get it out, so it’s kind of nice to have something that’s not really that stuck in there in case you ever got to get it out.
Ben James: I just thought about it, if you do cement it in, you have to get it out, what does that process look like?
Dr. Klug: It’s pain. Usually, it’s the same principles as the femur, but basically, if somebody has a cemented humeral component and it’s cemented all the way down, usually what you do is you do the same approach, you get down there. By the time you’re doing a second surgery, the shoulder is full of scar tissue, so you got to get rid of all that stuff too. In my opinion, you should probably find the axillary nerve because since the shoulder is now full of scar tissue, it might not be where it’s supposed to be. That’s your major catastrophic complication, is if you have an axillary nerve injury. I always find the axillary nerve and protect it.
Then basically you take the inserter that was used to put in the prosthesis and then you snap it back on there and then you just start whaling on it with a hammer and try to get the thing to pull out. Some of them have like a slap hammer, like a dent puller type thing, where it attaches to that. Some of them just have a big mallet and like a little anvil at the end of it, where you just sit there and whack the hell out of the thing and wait until it comes out. If that doesn’t work, then basically what you have to do is you have to split the humerus to get it out.
There’s ways, you can make windows in the humerus where you make a longitudinal cut and then, say, 5 millimeters or 8 millimeters away, you make another longitudinal cut and then connect the two at the bottom. You’re trying to make a window in the humerus without splitting it completely. By the way, you don’t split it all the way down, so the whole humerus doesn’t fully open like a book.
If you split it, you only split it, say, halfway down, which means you’re trying to get it to open just a little so you can get in here and in here to try to chip away the cement, but you’re talking about– The humerus is only 2 or 3 millimeters thick and the cement is a millimeter thick, so it really can be kind of a pain. Getting the things out is kind of a pain.
Ben James: I guess how often do you have to go in for a revision or a second surgery for shoulder replacement?
Dr. Klug: In my practice, I do it fairly regularly because I’m the guy around that does the bad shoulder stuff, so I’m the guy that does the revision stuff. Thankfully, I very rarely revise my stuff, but now that shoulder replacements are getting more common in the community, I’m doing a lot more revisions because somebody else either didn’t do it right or got it– The other thing that can happen is it can dislocate.
It dislocates because the soft tissue tension is not right. Usually, that means they put it in too loose. When the things come in different sizes, you can add height or length to the thing, but you can only add so much. If they put in, say, a +0 size spacer on there, which is part of the prosthesis, and you pop the thing apart and you put in a size +6, I mean you add six millimeters, and that keeps it stable and great, but if 6 is the biggest they’ve got and the patient needs a 12 or a 10, then you have to take the whole thing out and put it in a different place.
Ben James: I’m assuming that the outcome of the replacement afterwards is not as good as the first time?
Dr. Klug: You got it.
Ben James: Awesome. I know, we talked about this as well in the past, that you’ve done a little bit of design work yourself, do you want to touch briefly on what that looks like and what that came to today, [crosstalk] if you can?
Dr. Klug: It’s FDA approved, it’s patented all that stuff. It’s publicly available now. One of the things that happens in the shoulder, it helped to have a little diagram or something, is if you understand that the deltoid basically elevates the arm by pulling from the acromion, which is the bone above it, to the humerus, and the rotator cuff creates a fulcrum. One of the things that we learned years ago is that the humerus generally sticks out a little bit farther laterally than the acromion, so the deltoid wraps around it.
That part of the humerus is called the greater tuberosity, and the greater tuberosity has multiple functions, one of which is that’s the insertion of the rotator cuff or certain parts of the rotator cuff, but it also, because the deltoid wraps around it, it causes the deltoid to compress the humerus into the glenoid, which keeps it more stable, but it also helps with the fulcrum part of it.
The thing that we didn’t really realize until maybe 10 or 15 years ago, when we started doing reverse shoulder replacements, is some of the people that were getting reverse shoulder replacements, because it was the salvage procedure for all things bad on the shoulder, they were missing the top of the humerus, and they were missing the greater tuberosity.
There’s several things we found, one of which is if you did a reverse shoulder replacement on somebody that was missing the top of the humerus, there was a higher rate of dislocation. The second thing we found is, like earlier, I was saying that the reverse shoulder replacement makes it so you can elevate your arm almost all the time, some people don’t regain the ability to do overhead activities with a reverse shoulder replacement.
If you take somebody that’s missing the top of the humerus, there is a higher likelihood they will not regain overhead function. We started to ask why that is, and we started to realize that the greater tuberosity also creates this other thing, we call it deltoid wrap, which is, the deltoid, it goes from the acromion, it wraps around the greater tuberosity in order to insert on the humerus.
Basically, if you get rid of that bump, then the deltoid is not working as efficiently. When this research started coming out a long time ago, I looked at it and said, “Well, then it seems to make sense that we should make a prosthesis that has that for people that are missing it.” Most of the time, the humerus is intact, including the top of the humerus, so you just put the shoulder replacement in the humerus, and the greater tuberosity is there, but there are people with, say, for example, either bad fractures where the greater tuberosity is gone or it’s missing or they’ve had previous surgery, that has been excised, or they had a tumor or something like that.
Basically, I came up with this way of making a prosthetic greater tuberosity that mounts on the prosthesis. At that time, I was a consultant for a company, and I went to them and basically said, “Hey, I’ve got this idea,” et cetera. They looked at it, and I was sort of surprised that they bought it right away. They’re like, “That’s actually a pretty good idea.” I already had a design that I wanted to do, because the prostheses they made were left and right specific.
Basically what I was trying to do, because my old fellowship director in New York designed one of the most popular shoulder replacements, and I used to talk to him a lot about design stuff, et cetera. He would tell me about things like, one, you got to make it idiot-proof because everybody on the planet is going to try to take shortcuts and put it in wrong and then it’s going to make it look like the prosthesis doesn’t work.
Two, you have to put redundancy into the system. You have to make it so there’s– Like earlier when I was saying you got to cut the humerus, you can either put it in the humerus, you can put it on the humerus, you can do it this way, you can do it that way. That came from him.
Basically, his system had three different cutting guides in it. One, because some people just have different preferences, “I just like to do it this way or the other way,” but two, and more importantly, even though we don’t really talk about it, is that each way of doing it functions as a check to make sure the other way is done right. If you put on one cutting guide and it doesn’t look right and you put the other cutting guide on and it’s in the same place, then it’s probably right. If you put the other cutting guide on and it’s in the different place, then something is wrong. You use the redundancy in the system to basically check to see that you’re not screwing it up. The other thing that he used to talk about was inventory.
It’s nice to go and design things, but if you can design something that’s not left or right specific, then you can cut down half the shipping, half the inventory, half the [unintelligible 01:02:33] , half the packaging, all that other sort of stuff and the manufacturing, et cetera. The company that I was working with at that time had a shoulder replacement that I wanted to design this thing to mount on, but it was left and right specific.
Basically, what I did is I designed a greater tuberosity that would mount on their shoulder replacement, and their shoulder replacement had this thing that stuck off the side of it called a fin, which basically is just like a big piece of metal that sticks off the back. It was designed for fractures, and the location of that fin was designed to sit in the location of where the humerus usually fractures in those people that were getting that type of surgery.
The problem though is it’s not symmetric. The one on the left is in the corresponding location to the one on the right, but you can’t put a left prosthesis in the right shoulder because it’s in the wrong place. Essentially, what I did was I designed this implant that would mount to the fin, but I designed the implant to have two slots in it off-centered so the same implant could be used for left and right. Then basically there was just two set screws that went through it. The way it was threaded, one of them, the screw was threaded by the head of the screw, and the other one was threaded by the tip of the screw.
Since they’re both going in the same direction, basically if you did a left or a right, you just used the top screw for the bottom or the bottom screw for the top because they were symmetric, and they really liked the idea that I had already considered inventory, et cetera. We went through a few different design iterations, and it got changed, et cetera, but at least the idea survived, they ended up making left- and right-specific prostheses because they wanted to add some other stuff to it, et cetera, but it eventually came out, I don’t know, a couple of years ago, and it was on an early release.
Then one of the trials was recalled voluntarily because one of the screws in the trial wasn’t working even though the prosthesis was working, and they didn’t want people to put it in wrong because they didn’t have a good trial, so they did a voluntary recall of it maybe two years ago or something, I don’t know, maybe a year ago, and it’s been back maybe a year.
I got the official US patent on it, I think in June. It’s got a bunch of other patents. There’s a US patent, a Canadian patent, a European patent– I think there’s like nine of them. We had like six or seven of them already, and the US one came in somewhere around June of this year, and it’s been FDA approved for, I don’t know, three or five years. That happened a long time ago. That’s a whole another process, if you want to talk about that.
Unfortunately, there’s a lot of people that got a lot of good ideas, but nobody listens to them unless you have some kind of foot in the door with some company that’s interested. Thankfully, since I’d been doing a lot of shoulder replacements for a long time, I was already a consultant for several different companies on a fracture product and shoulder replacement, et cetera, I went to the company that I was working with on the shoulder replacement, that’s the guys that came out with it. That was the guys that were interested because I was already a part of their consulting team and teaching their courses and running their labs and that sort of stuff.
Ben James: Awesome. Really appreciate you being here today. Just want to wrap things up, I guess we talked about how the field of orthopedics, especially shoulder surgery has changed with the advent of the reverse over the past 20 years, I guess, where do you see the field of orthopedics moving and going forward over the next maybe 10 to 20 years?
Dr. Klug: What I really hope, I really wish some big entity like either the NIH or NSF or something like that would decide as a government that we really need to understand biologic treatment for stuff, PRP and stem cells, et cetera. As it is now, we have all these individual labs all over the place doing one project here and one project there and we don’t really know what to make of all this data, because a lot of it, one lab will say if you use PRP for tennis elbow, works great, and then another study will show that it doesn’t work.
To me, the big advancement that could be made in orthopedics over the next maybe 20 years would be biological treatments, stem cells, growth factors, all that other sort of stuff. You might find that a lot of the stuff that we do with implants and prostheses, we don’t even need them anymore because we can now replace the tissue or heal the tissue or repair the tissue, but I think we really need to understand that. I wish that there was more of a national, international push to do it.
Right now, a few people do it, but honestly, most of the people do it because it’s really expensive and it’s very profitable to do it, but nobody– I shouldn’t say nobody, but most of the guys that really do it are not interested in trying to figure out how it works, when it works, when it doesn’t work, what are the doses of this versus that, what is the timing of when the effect is, all this other sort of stuff that normally we leave that up to pharmaceutical companies to figure out the drugs and the dosages and the frequency and how long, do you take it for six weeks or do you only take one dose and et cetera, et cetera, et cetera.
In orthopedics, we’re in this surgical field which really could be made a lot more efficacious by treating it almost more like a pharmaceutical field. That’s where a lot of money is, and this stuff costs a lot of money, but there’s a lot of little projects here and there that are being done on it, but there’s nobody that’s really taken the bull by the horns and said, “I’m going to figure this out and know how this works, when it works, when it doesn’t work, what’s it for, what’s it not for, et cetera.”
Ben James: Interesting. Awesome. Once again, thank you Dr. Klug for being here today on the Biomechanics in the Wild podcast. Really appreciate it. Definitely learned a lot and hopefully the viewers learned a lot as well.
Dr. Klug: My pleasure.
Podcast Image: commons.wikimedia.org/wiki/File:X-ra…throplasty.jpg
Intro Music: Music by Music_Unlimited from Pixabay