When we think of building strong bones, most of us picture drinking plenty of milk for its calcium—at least, that’s what our elementary gym teachers used to tell us. But building and maintaining strong bones requires more than just calcium from milk; supplemental vitamins play a key role in the development and maintenance of strong bones. Bone fractures are common in young, but especially elderly people, and adding collagen supplements to one’s diet can have a major impact on bone toughness reducing the risk of fractures.
Continue reading “Taking Collagen and Copper Supplements can decrease the risk of bone fractures”Tag: sports injury
What are the RICE Method’s Impacts on the Healing Process Following Muscle Injuries?
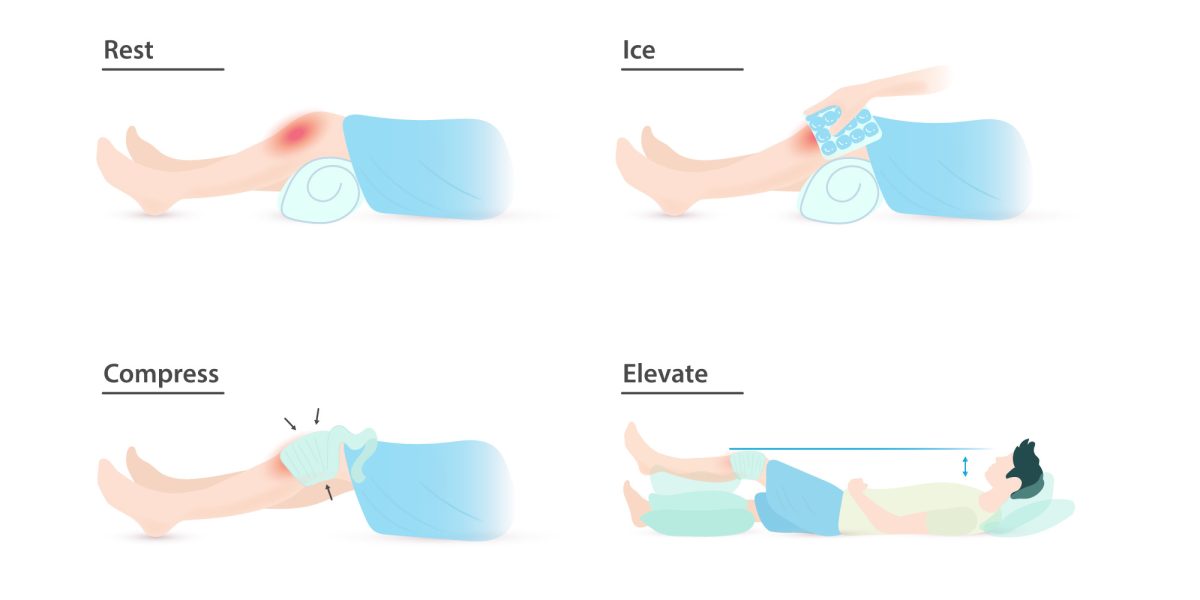
Have you ever been instructed to use the RICE protocol? Maybe you twisted your ankle on a root, slipped and fell hard on a patch of ice, or pulled your hamstring in an intramural soccer match. Rest, Ice, Compression, and Elevation is the common advice for immediate management of a soft tissue injury. But when you wrap a swollen calf, cover it with ice, and prop it on a pillow, what is actually going on beneath the skin? You may be able to feel the numbing cold of the ice and the compressive pressure of the wrap, but what about the healing processes that are harder to distinguish?
Continue reading “What are the RICE Method’s Impacts on the Healing Process Following Muscle Injuries?”Are We Fumbling the Ball on Player Safety?

Sports fans, especially those that watch college football (CFB) and the National Football League (NFL), are familiar with players going on “concussion protocol”. The consistent and often violent hits endured each game prompts the discussion of traumatic brain injuries players may experience trying to make a catch or tackle an opponent.
Continue reading “Are We Fumbling the Ball on Player Safety?”Dancers: Athletes or Artists?
Throughout history, there has been a long-standing debate about whether dancers should be classified as athletes or artists. Athletes need strength to be proficient in a sport. Artists require creativity to produce works of art. Dancers combine strength with artistry to not only leap high into the air but also look graceful as they do so. Yet, many people still refuse to classify dancers as athletes or even as athletic artists.
Continue reading “Dancers: Athletes or Artists?”Knee Pain from Golf? Look No Further.
If you like golf, you probably remember watching Tiger Woods win the 2008 U.S. Open with a torn anterior cruciate ligament (ACL). This may have seemed like a rare injury for a golfer, as most golf-related injuries involve the lower back, but knee injuries due to the golf swing are more common than you may think. In fact, the prevalence of knee injuries in golf is roughly 18%, with an even higher percentage when you only consider the elderly. Since most of these injuries are a result of overuse, it is important for golfers to understand why these injuries occur if they want to keep playing for years to come.
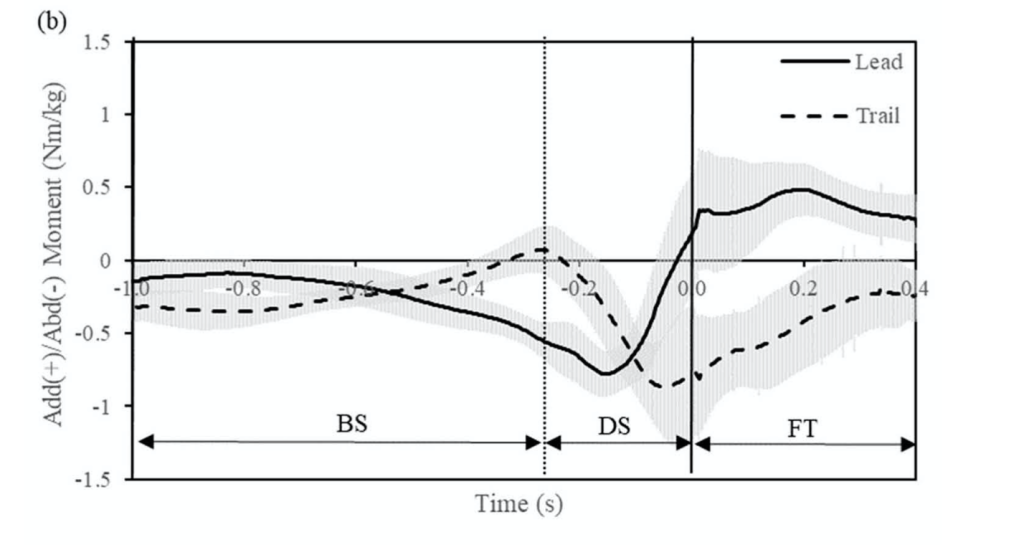
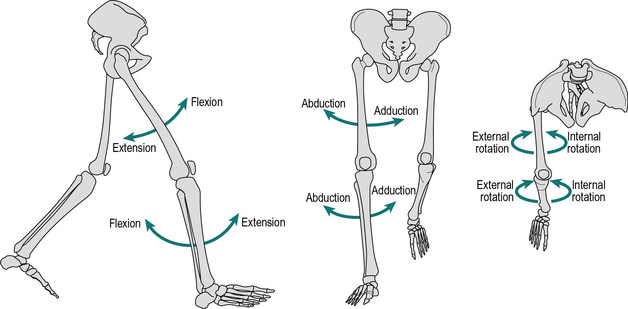
Read More: Knee Pain from Golf? Look No Further.Unlike traumatic injuries in high-intensity sports like football or basketball, most golf-related injuries are the result of overuse. As for the knee joint, there are multiple mechanical factors in the golf swing that contribute to overuse injuries. During the downswing, the lead knee rotates rapidly from a state of adduction (external rotation) to a state of abduction (internal rotation). This creates an abduction moment on the lead knee, which can cause ACL tears. The graph shows a plot of adduction/abduction moments on the knees during a golf swing, which was measured using force plates and retroreflective markers on golfers’ legs.
The magnitude (roughly 1 Nm/kg) is not large enough to cause traumatic stress on the ACL but is enough to potentially cause an injury over many repetitions of the golf swing. In addition to rapid rotation, the lead leg undergoes rapid extension during the downswing. The combination of these movements in large volumes over time can lead to other ligament tears or osteoarthritis. Osteoarthritis occurs when tissues in the joint break down over time.
In addition to these biomechanical movements, other factors like pre-existing knee conditions play a significant role in golf-related injuries. Over 30% of golfers with previous knee pain feel that golf has made their symptoms worse. The same is true for golfers with a previous total-knee arthroscopy (TKA), as nearly 34.9% experience pain after playing. Considering that golf is very popular among the older population, it is important to understand how to limit the risk of injury in the golf swing.
While the golf swing can lead to overuse injuries, there are a few preventative methods golfers can implement to protect their knees. Several studies recommend that golfers rotate their lead foot open (towards the target) by roughly 30 degrees. This decreases the stress on the medial (inner) side of the knee, a common area for osteoarthritis. Another adjustment golfers can make in their setup is how close/far they stand from the golf ball during the swing. Standing closer to the ball lowers the peak abduction moment on the lead knee, while standing farther away reduces the peak adduction moment. Depending on which area of your knee is in pain or has experienced previous injury, you may want to implement these adjustments to your setup. If you are experiencing pain on the inside of your knee, you should stand closer to the ball. Conversely, if your pain is on the outside of your knee, you should stand further away from the ball. Other preventative methods include warm-up stretching and regular exercise to activate and loosen the knee joint and surrounding muscles. If you’d like to learn more about these preventative methods, click here.
Bend it like Beckham?: Genu Varum (Bow Leg) in Soccer Players
Soccer, or football for those outside of the United States of America, is the most popular sport in the world, and its popularity is only rising. In the United States, although soccer is not the most popular sport, it is growing rapidly. Part of the reason behind this growth, around 20% American parents think soccer to be a safer sport for their children to play compared to American football. However, soccer players still suffer injuries.
Continue reading “Bend it like Beckham?: Genu Varum (Bow Leg) in Soccer Players”You’re En Pointe! Biomechanics and Ankle Injury Risk in Ballet Dancers
Dancing in pointe shoes raises the risk of injury for female ballerinas. Complex balletic movements require elevated muscular efforts and can put excessive stress loads on the ankle bones. Not many biomechanical studies focus on ballet, even as findings could contribute to decreased injury risk for dancers. A number of factors, such as ground reaction forces, ankle sway, and shoe flexibility can affect a dancer’s injury risk. But which factors contribute most?
Continue reading “You’re En Pointe! Biomechanics and Ankle Injury Risk in Ballet Dancers”Let Kids Be Kids: The Unnecessary Dangers of Youth Sports Specialization
The allure of athletic success is hard to ignore in today’s society. The opportunities, notoriety, and wealth that come along with prowess in a particular sport are certainly enticing and have contributed to a growing trend towards youth sports specialization, where athletes focus on one sport from a very young age. And while the work ethic of these young athletes is admirable, their reasoning and that of their parents is a bit flawed.
Continue reading “Let Kids Be Kids: The Unnecessary Dangers of Youth Sports Specialization”Why is heading the ball so dangerous for youth soccer players?
I received my first concussion while playing soccer at 15 when I was knocked out by a ball that was “accidentally” punted directly into the side of the head. It seemed to me like this was one of the few, rare ways to get a concussion from the sport – an unlikely occurrence combined with an unusually aggressive impact.
Continue reading “Why is heading the ball so dangerous for youth soccer players?”The Dangers of Using Your Head: The Biomechanics of Sports-Related Concussions
Anyone that has ever had the misfortune of banging their head know how painful it can be, but does everyone understand just how dangerous it can be? Concussions occur when the brain hits the interior walls of the skull, either due to a direct blow or a sudden start or stop. These brain injuries most often result in confusion, headaches, and loss of memory but more severe injuries can cause vomiting, blurry vision, and loss of consciousness. In rare instances, they can even cause a brain bleed and result in death. Repeated concussions can lead to neurocognitive and neuropsychiatric changes later in life as well as increase a person’s risk of developing neurodegenerative diseases like Alzheimer’s.
Continue reading “The Dangers of Using Your Head: The Biomechanics of Sports-Related Concussions”