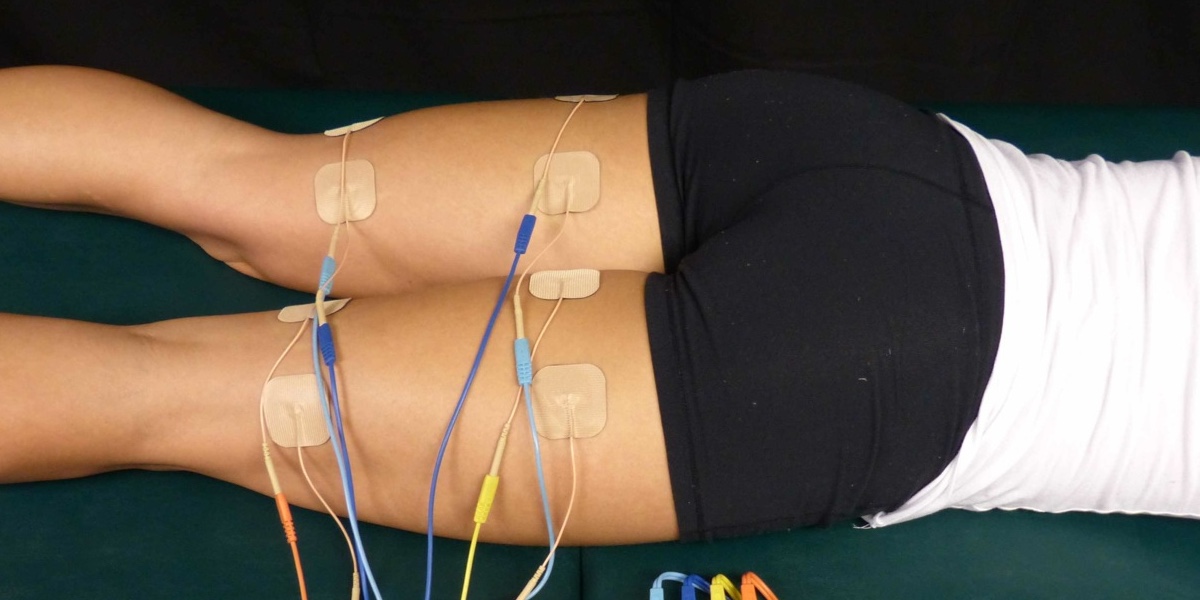
Power to many is control, electricity, or strength depending on what one is talking about. But to muscles, it involves all three. When at the gym and thinking that someone looks powerful they usually have a lot of muscle. However, to control or activate all that muscle and use their strength it requires electrical power.
Continue reading “Power in Muscles”Tag: recovery and rehabilitation
What are the RICE Method’s Impacts on the Healing Process Following Muscle Injuries?
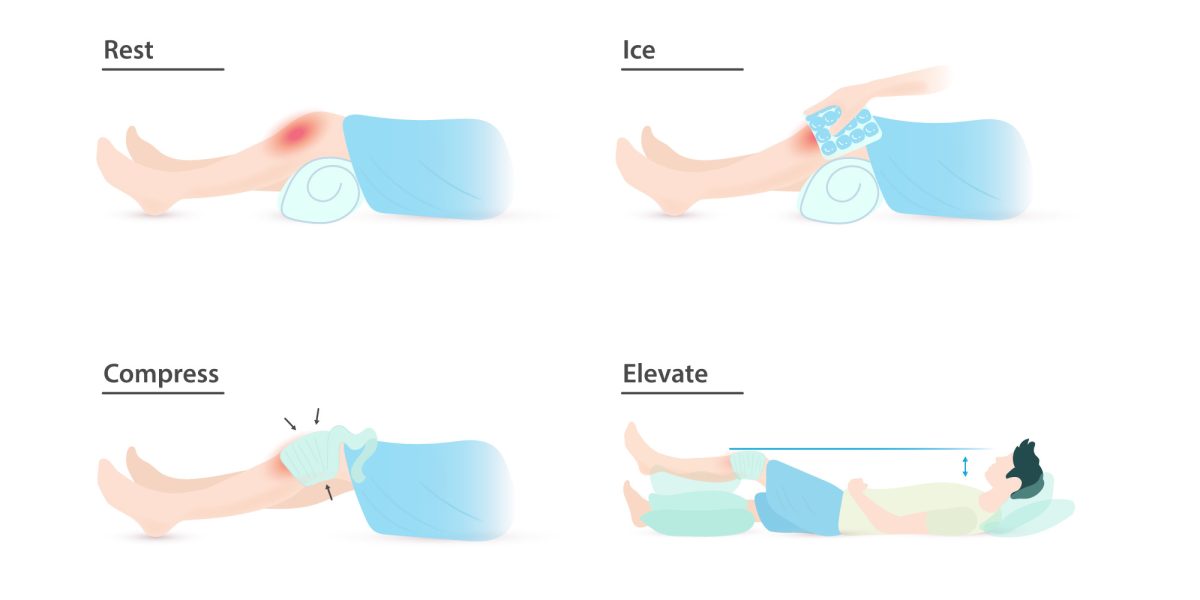
Have you ever been instructed to use the RICE protocol? Maybe you twisted your ankle on a root, slipped and fell hard on a patch of ice, or pulled your hamstring in an intramural soccer match. Rest, Ice, Compression, and Elevation is the common advice for immediate management of a soft tissue injury. But when you wrap a swollen calf, cover it with ice, and prop it on a pillow, what is actually going on beneath the skin? You may be able to feel the numbing cold of the ice and the compressive pressure of the wrap, but what about the healing processes that are harder to distinguish?
Continue reading “What are the RICE Method’s Impacts on the Healing Process Following Muscle Injuries?”The Science Behind Load Management: How Isometrically Overloading Tired Knees Can Promote Growth and Healing
Many athletes who experience pain right below the kneecap after a spike in volume of explosive physical activities (ie. running/jumping) are diagnosed with patellar tendonitis, commonly referred to as runner’s or jumper’s knee. The suffix “itis” is Greek for inflammation and a common remedy is rest to reduce the inflammation. In some cases, an initial rest period combined with physical therapy to strengthen surrounding muscles such as the hip flexors and gluteus medius is enough to alleviate the knee pain for good, in other cases the rest is of no benefit or even worsens the patellar tendon’s condition and starts a chronic cycle of resting and then returning to activity in more pain than before. In these cases a more accurate diagnosis of patellar tendinopathy is correct. Patellar tendinopathy implies chronically recurring pain on the anterior of the knee that is difficult to treat. In such cases, an MRI often reveals small lesions throughout the patellar tendon indicating that the tendon is structurally damaged and not just inflamed. A better understanding of the patellar tendon’s biological composition, and biomechanical function may help to resolve future cases of patellar tendinopathy.
Continue reading “The Science Behind Load Management: How Isometrically Overloading Tired Knees Can Promote Growth and Healing”Egan Mills and Blake Kusky Discuss Eccentric vs Concentric Weight Training
Bodily movement without eccentric and concentric motion is impossible. When it comes to weight/strength training, the portion of the movement that tends to be more focused on is the concentric portion. In this analysis, the effects of both eccentric and concentric weight/strength training will be fully fleshed out with both their positive and negative results.
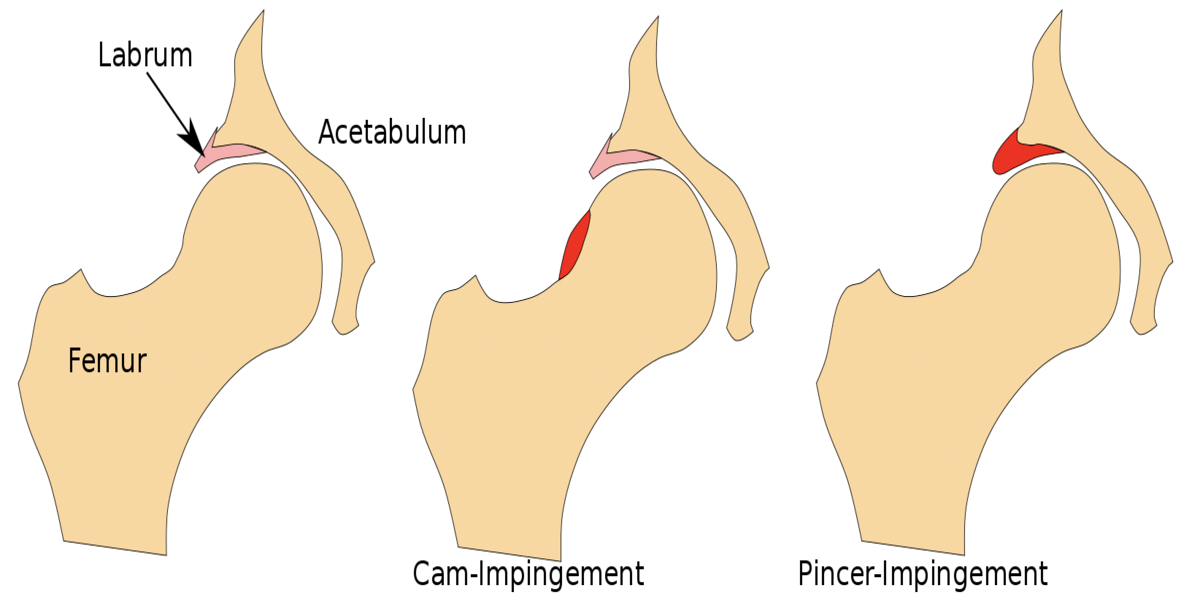
Hip Hip Hooray: Joint Functionality Can Be Restored After Hip Labral Tear
Do you experience deep, sharp pain in your groin? Or a feeling of “catching” or “popping” in your hip joint as you go about your daily activities? Is your range of motion you once had now severely limited? If so, you could be experiencing symptoms of a hip acetabular labrum tear, an ever-increasing problem in society that fortunately, has effective treatments.
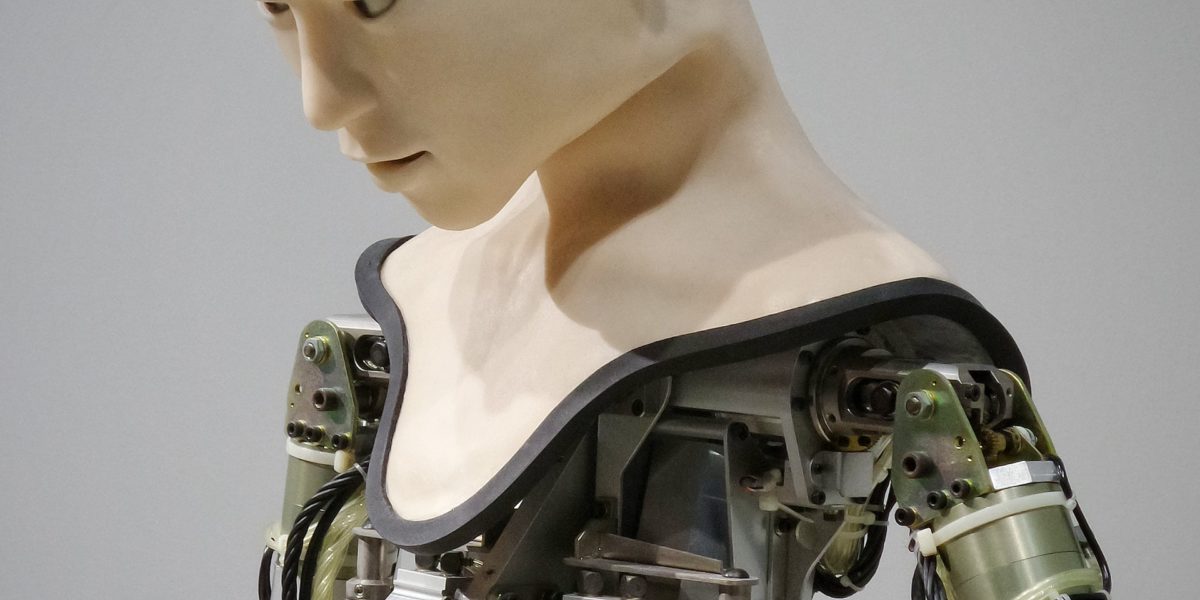
Continue reading “Hip Hip Hooray: Joint Functionality Can Be Restored After Hip Labral Tear”What’s Good in Robotic Post-Stroke Rehabilitation Therapy
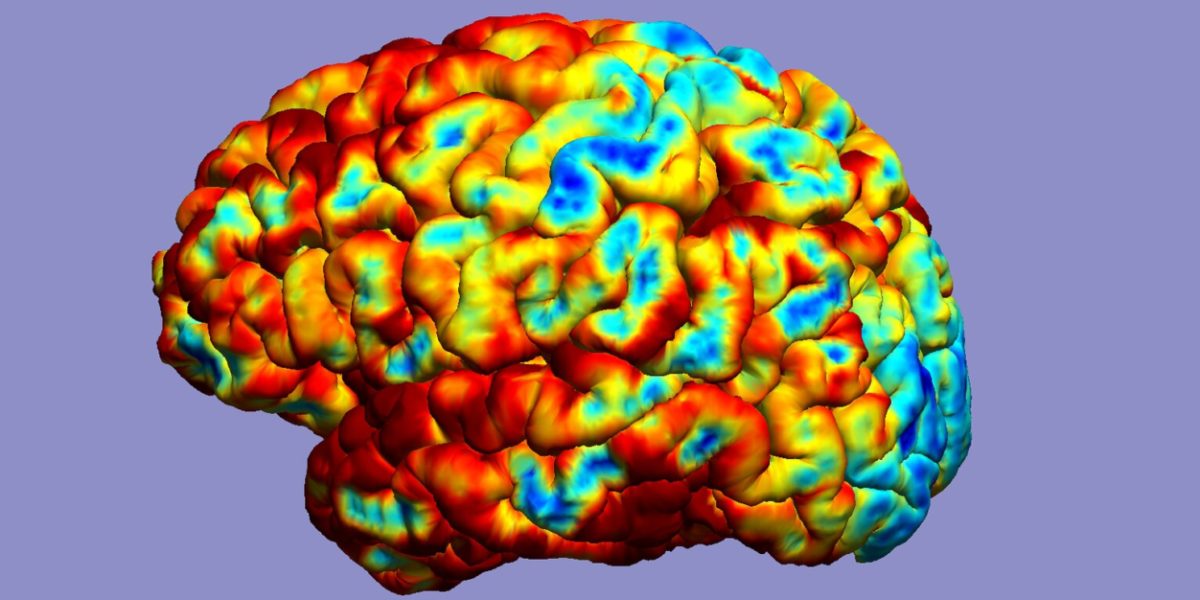
As medicine progresses, the quality of life improves for everyone, resulting in more people living longer. Unfortunately, as a result of an increasing number of people living longer, the number of stroke victims has increased as well. A stroke is a disease that affects blood flow to and inside the brain, causing the loss of movement and control in parts of the body. This loss of control leaves stroke victims very dependent on relying on others to help live a normal life.
Continue reading “What’s Good in Robotic Post-Stroke Rehabilitation Therapy”The Ultimate 2-for-1: the Power of Contralateral Strength Training
For the competitive athlete, injury often means loss. Loss of playing time, loss of skill development, and most importantly, loss of training time. These are all unfortunate consequence of getting a bone or tissue injury requiring a long-term healing prognosis. Injuries can be so devastating because the road to recovery is often times an arduous two-step process. First, the athlete must wait for their broken bones, torn ligaments, or pulled muscles to naturally heal. During this time, the athlete’s injured limb is likely immobilized in a cast or brace, leaving the resulting muscle to slowly atrophy as the body tries to heal itself. As a result, an athlete must spend the second part of their recovery process re-training the weakened muscles in the immobilized limb to return to full-strength. What if there was a way to heal and train the body at the same time? This is the power of a neurophysiological phenomenon known as “contralateral strength training.”
Continue reading “The Ultimate 2-for-1: the Power of Contralateral Strength Training”A Second Chance: Robotic Exoskeletons May Be the Future of Mobility for Patients with Spinal Cord Injuries
No one ever imagines themselves getting seriously injured. Accidents do happen though, like car crashes and unexpected sports injuries. These events can drastically change a person’s life, leaving them unable to perform simple daily tasks without assistance, such as walking. One injury that can radically impact a person’s life is a spinal cord injury. There are approximately a quarter of a million people in the United States with spinal cord injuries, and that number grows by 12,500 each year.
Continue reading “A Second Chance: Robotic Exoskeletons May Be the Future of Mobility for Patients with Spinal Cord Injuries”Oops I Did It Again: The Biomechanics Behind Repetitive Ankle Injuries
Ankle injuries – either sprains or fractures – are one of the most common sports traumas plaguing the US today. Sprains are overextensions or tears in ligaments. Fractures, on the other hand, are broken bones.
Continue reading “Oops I Did It Again: The Biomechanics Behind Repetitive Ankle Injuries”Soft Robotics: Humanizing the Mechanical
In media and science-fiction, robots have stereotypically, and perhaps somewhat unfairly, been depicted as mechanical, stiff assemblies of moving joints and complicated circuitry. While this still holds true for many robots designed today, whether for industry or research, the past few years have seen a growing interest in soft robotics in academia, industry, and popular culture. As the name implies, many research groups have begun investing in constructing robots from compliant, softer materials.
Continue reading “Soft Robotics: Humanizing the Mechanical”