Typically, the joys of childhood that adults reminisce about include carefree playing, running, and jumping—not cancer. Despite this, childhood cancer affects nearly 10,000 children in the U.S. every year, and of these cases, about 500 (2 percent) involve osteosarcoma. Rotationplasty is a surgery that can give childhood osteosarcoma survivors requiring amputation the best chance of running and jumping again, just like before.
Read more: Your ankle could replace your knee! – How Rotationplasty gives ankles new function. Continue reading “Your ankle could replace your knee! – How Rotationplasty gives ankles new function.”Tag: surgery
Using Vacuum Pressure to Heal Stroke & DVT Patients
Blocked blood vessels
Strokes are the 2nd leading cause of death worldwide. An estimated 795,000 people suffer a stroke every year in the United States. A stroke occurs when a blockage in a blood vessel leads to disruption or blockage of blood flow to the brain. Also, an estimated 350,000 people every year in the US suffer a deep vein thrombosis, which is when a blood clot forms in the deep veins often in the lower extremities. Venous clots can travel up the legs into the lungs or other vital organs, where they can become extremely dangerous or even fatal. When a blood vessel in a vital organ becomes occluded, blood flow must be restored as quickly as possible to return the patient to health.
There are two main procedural methods for removing blood clots from blocked arteries and veins: using tooling to extract the clot mechanically or using pressurized instruments to suck the clot mass out. Suction thrombectomies, also known as aspiration thrombectomies, are becoming more common because they have higher success rates of patient recovery.
READ MOREOsseointegrated Prosthetic Devices: What Are They and How Did We Get Here?
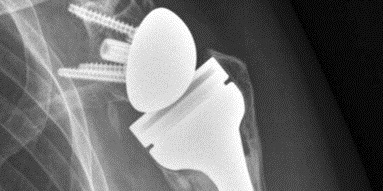
Prosthetic devices have been an option for limb-different individuals for thousands of years. Over the centuries, there have been countless discoveries that have led to the modern prosthetic leg. Today’s customary prosthetic leg is comprised of two main components: the socket and the device itself. The socket is often made of carbon fiber and is molded to the contours of the user’s residual limb. This socket is directly connected to the device itself, which includes an ankle and possible knee joint depending on the length of the limb. The socket serves as the connection point between the user’s residual limb and the prosthetic leg.
Continue reading “Osseointegrated Prosthetic Devices: What Are They and How Did We Get Here?”Orthopedics and Shoulder Replacement (w/ Dr. Raymond Klug)
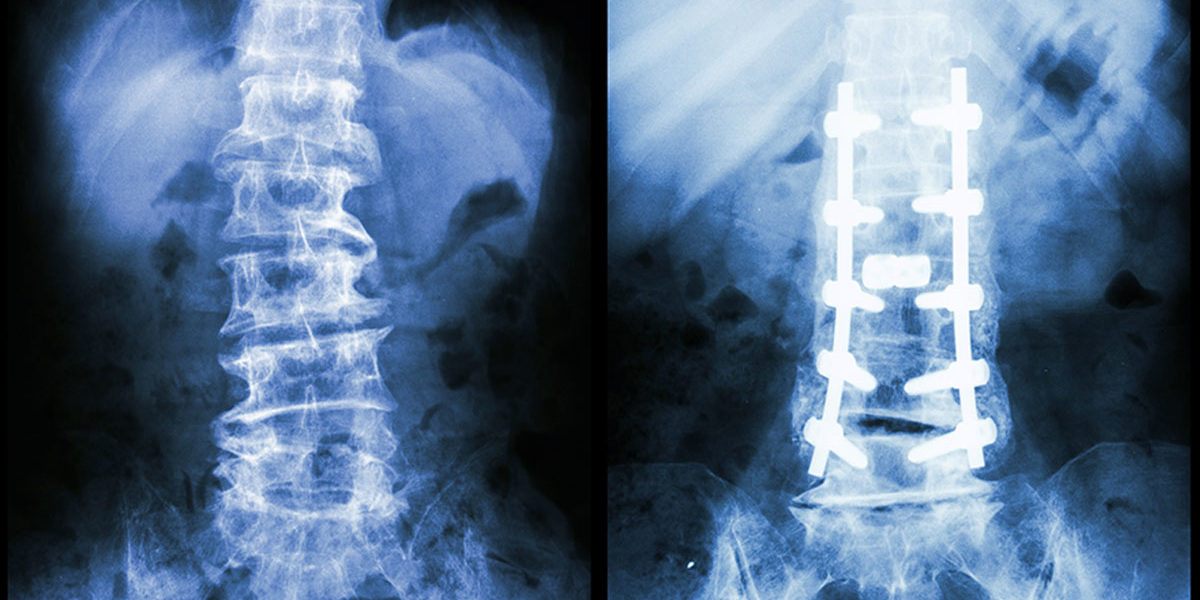
Strengthening the Spine with Pedicle Screws
How are pedicle screws being used to strengthen the vertebrae in spinal fusion surgeries?
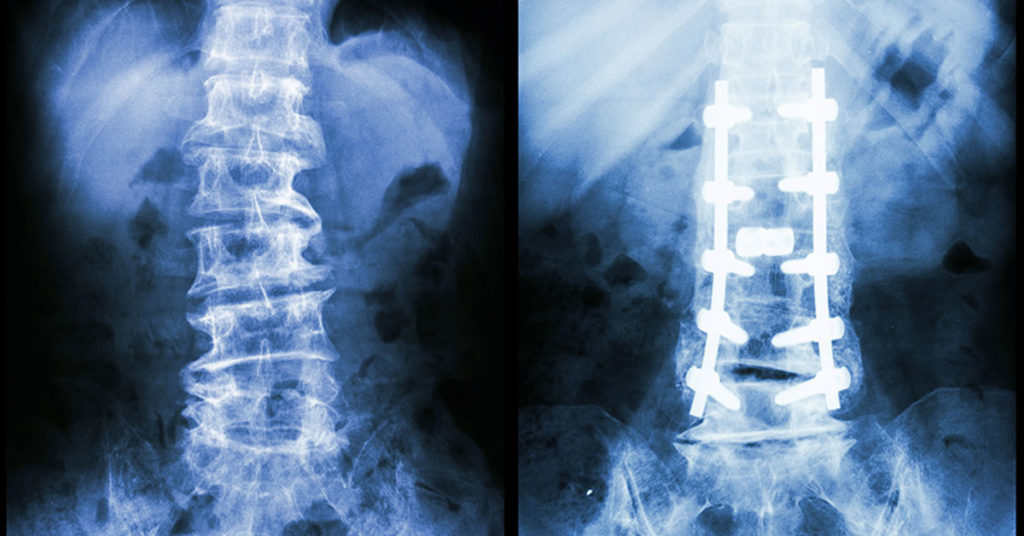
In the US alone, over 300,000 spinal fusion surgeries are performed every year to correct for fractures, deformations, or spinal instabilities. These surgeries are often performed by inserting a pedicle screw into the damaged vertebrae to increase the strength of the fusion. These screws are most often used in cases where the bone in the surrounding area is already weak, which decreases the likelihood of success in the surgery. Essentially, pedicle screws are used in damaged bones to increase their strength, in turn increasing the likelihood of success in a high-risk patient.
Continue reading “Strengthening the Spine with Pedicle Screws”Twists and Curves: Spinal Analysis and the Correction of Scoliosis
For anyone who had braces as a kid, you know how miserable the process can be. From rubber bands to the restrictions on what foods you could enjoy, having braces was a real pain. However, once the braces came off, it was all worth it to have perfectly straight teeth. While many adolescents go through orthodontic bracing to straighten crooked teeth, there are some who go through a similar process to correct the curvature of their spines.
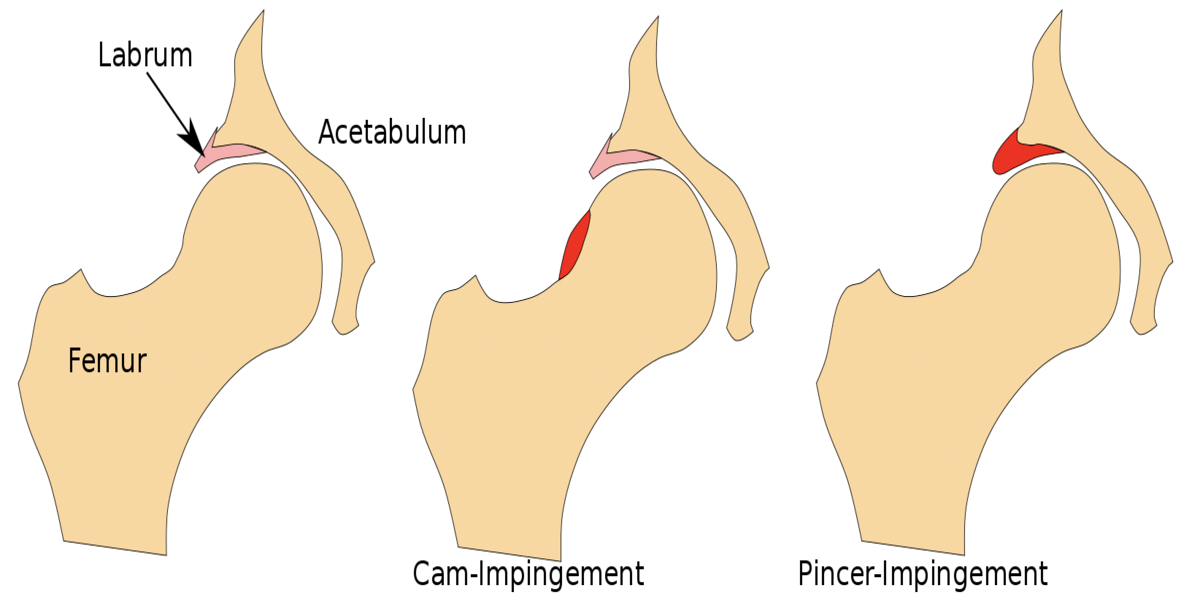
Hip Hip Hooray: Joint Functionality Can Be Restored After Hip Labral Tear
Do you experience deep, sharp pain in your groin? Or a feeling of “catching” or “popping” in your hip joint as you go about your daily activities? Is your range of motion you once had now severely limited? If so, you could be experiencing symptoms of a hip acetabular labrum tear, an ever-increasing problem in society that fortunately, has effective treatments.
Continue reading “Hip Hip Hooray: Joint Functionality Can Be Restored After Hip Labral Tear”What Can Different Types of Facial Wrinkles Tell Us?

Few people enjoy having wrinkles. Some people spend a lot of time, money and efforts trying to reduce the wrinkles on their face, while others simply appreciate them as something naturally occurs with aging. Regardless, wrinkles are always associated with aging. However, if we look into what different types of wrinkles are and how they form, we will find that not all wrinkles are bad. Not all wrinkles are caused by aging, and not all wrinkles should be treated the same way. Here, we introduce different types of facial wrinkles categorized by plastic surgeon and their corresponding treatment.
Continue reading “What Can Different Types of Facial Wrinkles Tell Us?”This Toner Might Be More Expensive: 3-D Printing Artificial Organs
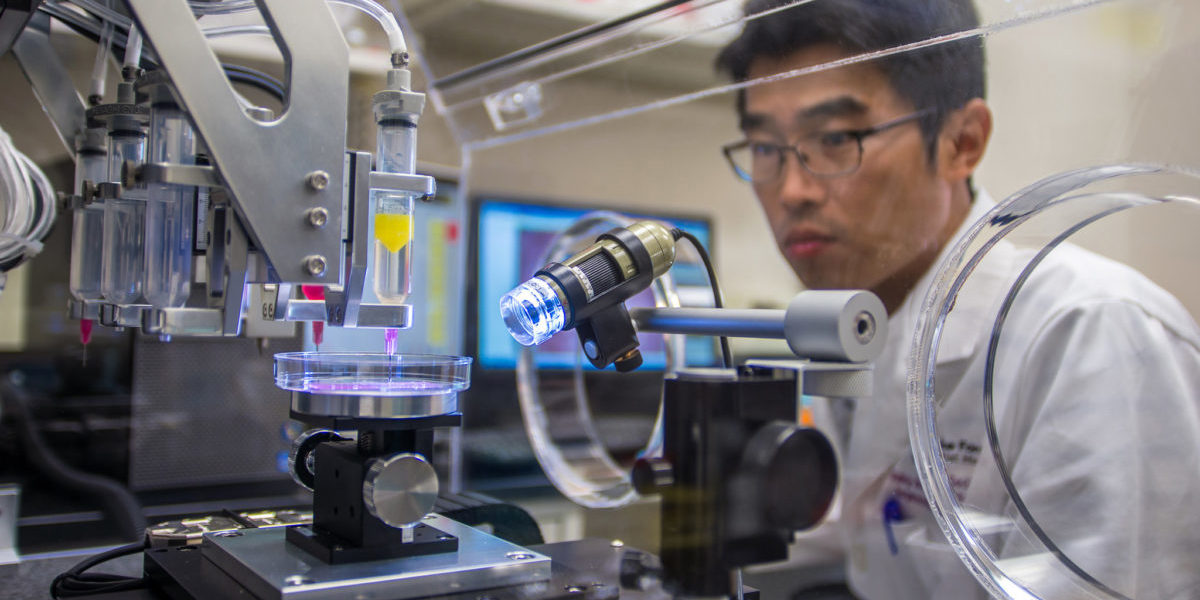
For most people in the United States who need an organ transplant, they will need to wait an average of three to five years on a list before they can get a lifesaving surgery. On average, 20 people die daily waiting on this list. There is a possibility of being able to bypass the wait time by manufacturing the required organs with 3D printing. This manufacturing technique was first used in the medical field for prosthetics and surgery practice models, with a goal to create fully functioning organs for those in need. Instead of using plastic or printer ink, the 3D printer uses cells to create biological constructions.
Continue reading “This Toner Might Be More Expensive: 3-D Printing Artificial Organs”Tearing and repairing the meniscus
How does someone go from being the youngest NBA MVP one year to barely making headlines the next? Ask Derrick Rose. After being named the youngest MVP in the NBA, Derrick Rose tears his ACL the next year and then tears his right meniscus twice in the span of three years. Knee injuries have not been kind to Derick Rose, but how does one tear their meniscus and how does it get repaired?
Continue reading “Tearing and repairing the meniscus”