Featured image courtesy of InjuryMap.
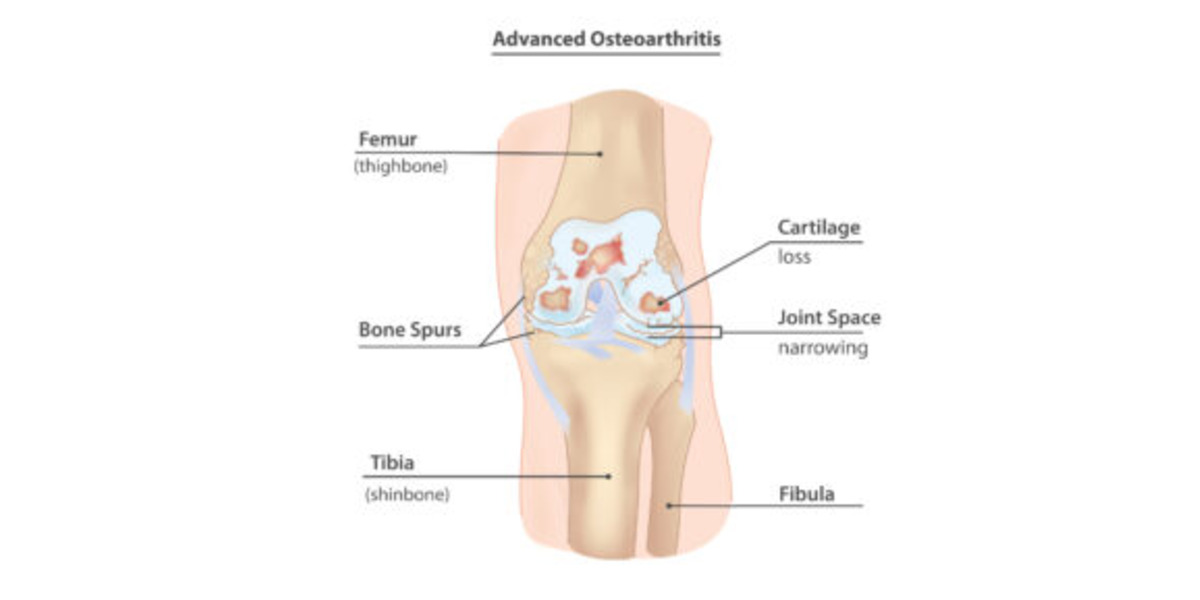
Joint degenerative diseases, such as Osteoarthritis, are an increasing cause of pain and disability in millions of people worldwide, per Sanchez-Adams et. al. As a culture of intense, nonstop work is promoted, people incline to not give their bodies enough time to rest, which has increased the cases of joint injuries, especially those to the lower body; specifically in those populations that are exposed to high intensity physical activity. This is concerning, since it has been discovered that joint injuries provoke an alteration in how these joints distribute loads, drifting from their physiological, or typical/natural, behavior, as demonstrated by Ko et. al. Consequently, this affects the biological response of the bone and cartilage that compose that affected joint, leading to potential degeneration due to the altered mechanotransduction (interpretation of mechanical signals to biochemical ones) interactions of the cell and cartilage forming cells, osteocytes and chondrocytes. This degeneration is what characterizes the concerning and debilitating Osteoarthritis (OA). This leads us to our questions: Why does the altered loading affect my joints? If I suffer an injury, can I prevent the degeneration of my joints and live a long, healthy life?
Continue Reading