Imagine this: you’re jolted awake in the dead of night, disoriented and feeling a sharp, relentless pain radiating through your lower abdomen. Glancing at the clock, it’s only 3 a.m., but you already know the culprit. Your period has arrived—along with the familiar, sometimes debilitating cramps that will have you reaching for ibuprofen every few hours just to make it through the day. For as high as 45-95% of people who menstruate, this monthly pain feels inevitable, with studies showing that dysmenorrhea is one of the most common gynecological conditions. In this post, we’ll explore the biomechanics of period cramps, diving into what’s causing that pain, how your muscles and nerves are involved, and ways to find relief.
Continue reading “Cramping My Style: The Biomechanics Behind Period Pain”Tag: pain
Balancing the Load: Understanding Pressure Distribution in Prosthetic Sockets
How do pressure profiles and shear stresses in prosthetic sockets affect prosthesis user comfort? For prosthesis users, comfort is essential for mobility, quality of life, and long-term health. The fit and alignment of a prosthesis are highly individualized and crucial for instilling confidence in daily activities. However, current prosthesis fittings are largely subjective, depending on the prosthetist’s experience and user feedback. This qualitative method often overlooks the critical factor of pressure distribution within the socket, which can significantly impact pain levels and ease of movement.
Read more: Balancing the Load: Understanding Pressure Distribution in Prosthetic Sockets Continue reading “Balancing the Load: Understanding Pressure Distribution in Prosthetic Sockets”Why Do Your Fingers Make A “Pop” Noise When You Crack Your Knuckles?
When cracking your knuckles, one tends to hear a “pop” noise that is loud, sharp, and irritating to most. This noise can be addicting in the sense that it makes others want to crack their knuckles. The main questions that I focused my research on were “Does cracking your knuckles or joints cause potential health issues for your future?” and “ Why does cracking a joint such as your knuckles make a “pop” noise?”
Continue reading “Why Do Your Fingers Make A “Pop” Noise When You Crack Your Knuckles?”Is my cell phone causing me neck pain?

77% percent of people in the world have a smartphone according to researchers. The most popular form of communication is text messaging. On average, people are spending 3-6 hours per day on their phone. Children are getting their first smartphones earlier and earlier. The unique capabilities provided by this technology are unmatched, but at what cost?
Continue reading “Is my cell phone causing me neck pain?”Pressurized Vessels Supporting the Spine: Structure and Function of Intervertebral Discs
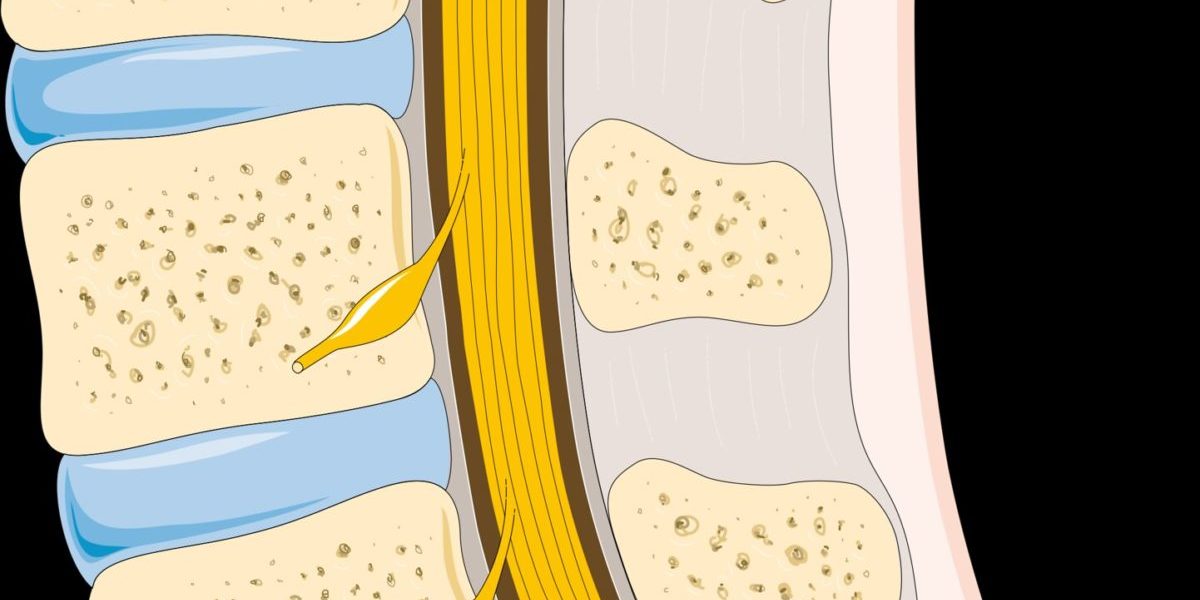
Back in 1989, it was estimated that about 2.5 million U.S. workers suffered from low back pain, and low back pain has even been talked about as one of the largest causes of disability in the world. Intervertebral disc degeneration is one of the most common reasons for low back pain in adults. In order to understand how disc degeneration occurs and causes pain, it is important to examine the structure and function of discs in the back.
Continue reading “Pressurized Vessels Supporting the Spine: Structure and Function of Intervertebral Discs”Hell for your Heels: Plantar Fasciitis and Heel Spurs
Heel and foot pain are somewhat universal issues, impacting people of all different sizes and activity levels. This type of pain can be seen in obese people, who have increased strain on their feet and heels. This pain can limit their mobility, and even discourage healthy amounts of exercise. It is also common to extremely active people, such as runners or sports players. This type of pain can prevent a person from participating in the athletics that they work so hard to compete in. I experienced a great deal of heel pain during high school, which made it difficult for me to play sports such as soccer, basketball, and track and field. This was an issue I had to deal with throughout high school, however I never understood what caused this pain that kept me on the sidelines at times.
Continue reading “Hell for your Heels: Plantar Fasciitis and Heel Spurs”Ways to Prevent and Treat a Common Annoyance: Headaches
Headaches can range from a mild annoyance to a debilitating condition that results in the inability to complete simple daily tasks. Odds are you have experienced a headache since about 50% of the population has suffered some type of headache. While there are many different variables that may have triggered it (injury, stress, chemical imbalances, etc.), the resulting symptoms are always negative. Scientists have been investigating what causes different types of headaches in hopes that they can help people prevent their occurrence and mitigate their symptoms.
Continue reading “Ways to Prevent and Treat a Common Annoyance: Headaches”Runner’s Knee: Knee Pain Isn’t Just for Old People
Don’t knee problems only plague old people or people who have run for a lifetime? I questioned this when, for the seventh time in a row, my knee was hurting only a mile and a half into my run. I’m too young for this! However, a plethora of information suggests that knee pain is perhaps not so uncommon in younger runners and athletes as I thought.
Continue reading “Runner’s Knee: Knee Pain Isn’t Just for Old People”Why your Muscles Hurt after a Workout
How often do we cut our overly ambitious workouts short because of exhaustion or muscle soreness? Probably more than we care to admit. But have you ever stopped to ask yourself why your muscles hurt, especially a day or two after your workout? The simple answer is, you’ve put so much strain on your muscles that you aren’t used to, so they tore, and now your body has to repair the tears and build up more muscle, so the same thing doesn’t happen in the future.
Continue reading “Why your Muscles Hurt after a Workout”