What would you do if you went to the doctor expecting to get back to work, only to be told you might not ever be able to go back to work again?
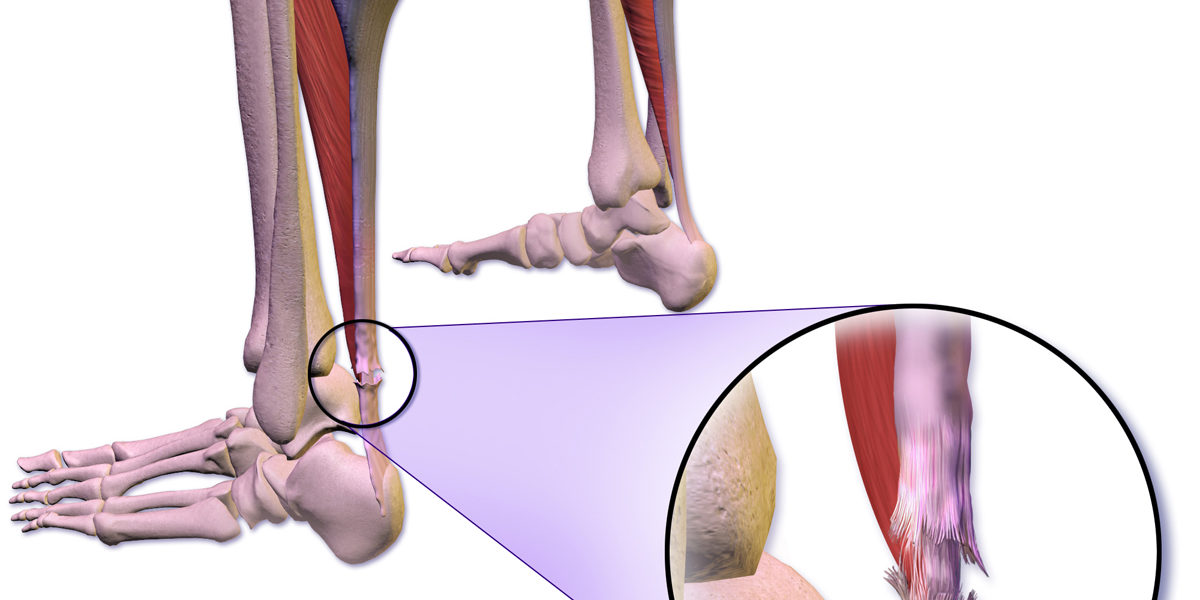
According to ESPN, on February 4, John Wall visited his doctor regarding an infection in his heel after a previous operation. The doctor checked the infection, but upon further analysis, realized that Wall had suffered a partial Achilles tear. Unlike former teammate Boogie Cousins, he did not suffer the tear on the court, but at home. It was reported that while at home he fell and experienced extra discomfort in his heel. His doctor reported that he will undergo surgery and will likely rehab for the next 11 to 15 months.
Continue reading “Back Against the (John) Wall”






![Walk [Under] Water: The Benefits of Underwater Running](https://sites.nd.edu/biomechanics-in-the-wild/files/2019/03/hydrotrack-e1680741443448-1200x600.jpg)