Ankle injuries – either sprains or fractures – are one of the most common sports traumas plaguing the US today. Sprains are overextensions or tears in ligaments. Fractures, on the other hand, are broken bones.
Continue reading “Oops I Did It Again: The Biomechanics Behind Repetitive Ankle Injuries”Tag: sports injury
Work Smarter Not Harder!
We have all likely heard the saying, “Work smarter not harder.” While this is generally referenced in an academic setting, it is also very applicable in athletics! One of the benefits to being a runner is that it’s a sport people can participate in at any age and nearly anywhere. Unfortunately, however, anywhere from 65-80% of runners get injured in a given year. A large portion of these injuries are related to overuse.
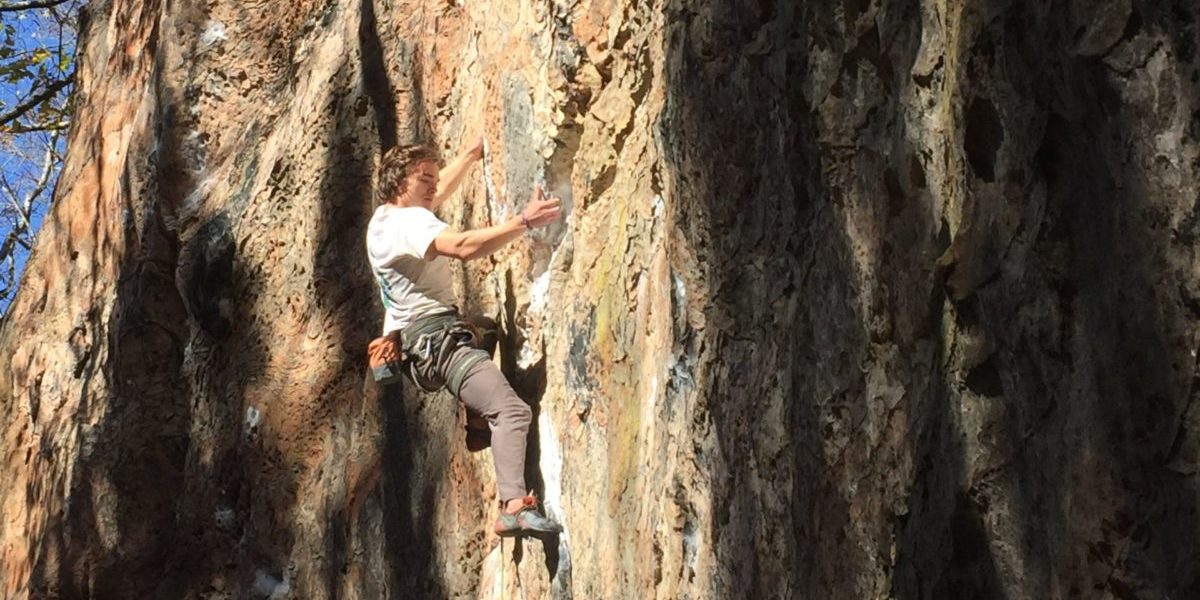
Continue reading “Work Smarter Not Harder!”Rock on, Dude!
In the rock climbing world, there is not much that people fear more than the sound of a “pop” coming from their fingers. That sound means months of rehab and can keep you off the rock for up to six months. But what exactly is happening when you hear that dreaded sound? The fingers are so small, how can one injury to the fingers be so devastating? Let’s dive in.
Continue reading “Rock on, Dude!”Ankle Sprains: An Epidemic in the World of Athletics
Have you ever been out running on a gorgeous fall day, only to have the run cut short by a painful misstep on a tree root covered by leaves? I have, and let me tell you – it’s awful! And even if you aren’t a runner, according to the Sports Medicine Research Manual, ankle sprains are a common, if not the most common, injury for sports involving lower body movements. Now, the solution to preventing this painful and annoying injury could be as simple as avoiding tree roots and uneven ground, but the real problem behind ankle sprains deals with the anatomy of the ankle.
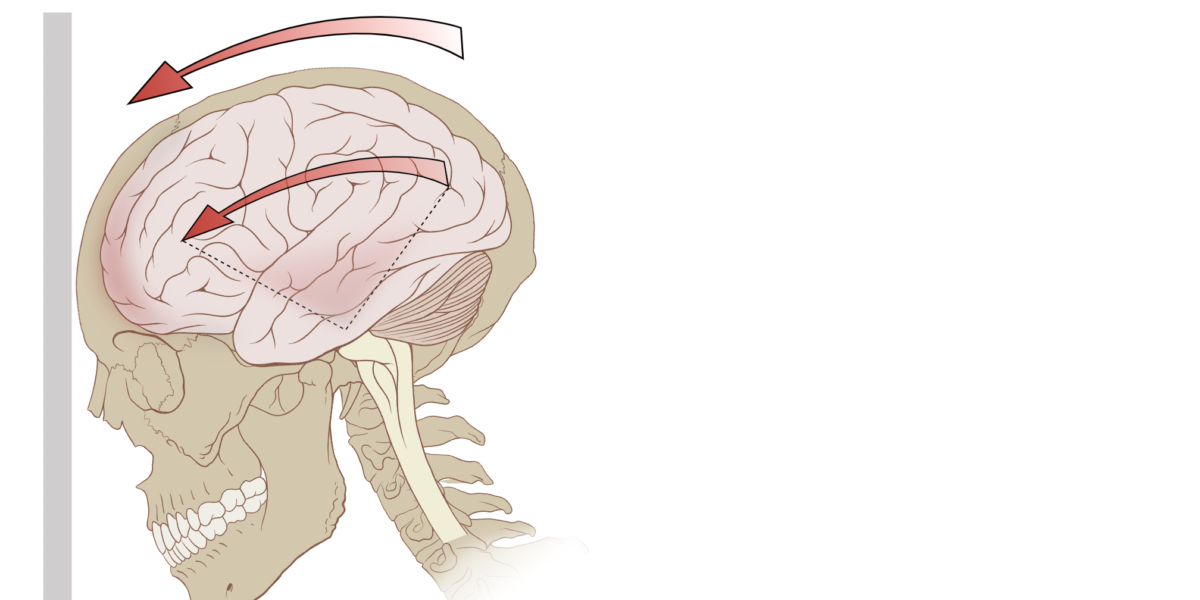
Continue reading “Ankle Sprains: An Epidemic in the World of Athletics”Attempting to “Knock Out” the Causes of Concussions
Approximately every 15 seconds, a traumatic brain injury occurs in the U.S. A concussion is a form of mild traumatic brain injury produced by a contact or inertial force to the head (or neck) area. A concussion causes the brain to rapidly move around inside the skull, harming natural brain function. According to the Brain Injury Research Institute, roughly 1.6 to 3.8 million concussions occur each year in the U.S., resulting from both recreation and sports related incidents. In fact, brain injuries cause more deaths than any other sports injury.
Continue reading “Attempting to “Knock Out” the Causes of Concussions”Using K-Motion Technology to Achieve the Perfect Baseball Swing
The question on every baseball player’s mind is: besides more practice, how can I improve my batting skills?
Continue reading “Using K-Motion Technology to Achieve the Perfect Baseball Swing”Tearing and repairing the meniscus
How does someone go from being the youngest NBA MVP one year to barely making headlines the next? Ask Derrick Rose. After being named the youngest MVP in the NBA, Derrick Rose tears his ACL the next year and then tears his right meniscus twice in the span of three years. Knee injuries have not been kind to Derick Rose, but how does one tear their meniscus and how does it get repaired?
Continue reading “Tearing and repairing the meniscus”What is Tommy John surgery?
In July of 1974, Tommy John, pitcher for the Los Angeles Dodgers, felt a twinge in his throwing arm, and could no longer pitch. Dr. Frank Jobe tried a new kind of surgery on John’s elbow, and after missing only one season, Tommy John returned to the mound in 1976 and continued pitching until 1989.
How?
Continue reading “What is Tommy John surgery?”What Makes Someone More Likely to Tear Their UCL?
It takes a lot to make a professional athlete collapse to the ground during a game. After throwing a pitch on September 14, 2019, Toronto Blue Jays pitcher Tim Mayza knelt on the side of the mound while clutching his arm, expecting the worst. The next day, MRI revealed that what he had feared: Mayza had torn his Ulnar Collateral Ligament (UCL).
Continue reading “What Makes Someone More Likely to Tear Their UCL?”What an Optimized Running Gait Can Do for You
Running is one of the oldest and most common forms of exercise, but there are many ways that running mechanics vary from person to person. Identifying the different running gaits is important so that their efficiencies and effects on the body can be analyzed. Injuries in runners are common and having an understanding of how different gaits apply stresses on the body differently can be used to educate runners on how to run in a way that will reduce the risk of injury.
Continue reading “What an Optimized Running Gait Can Do for You”