How are pedicle screws being used to strengthen the vertebrae in spinal fusion surgeries?
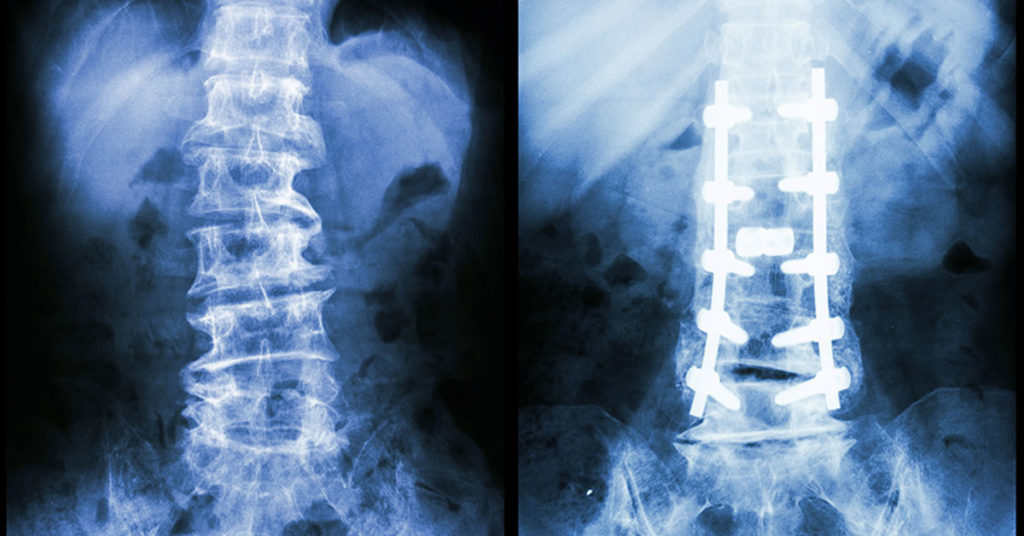
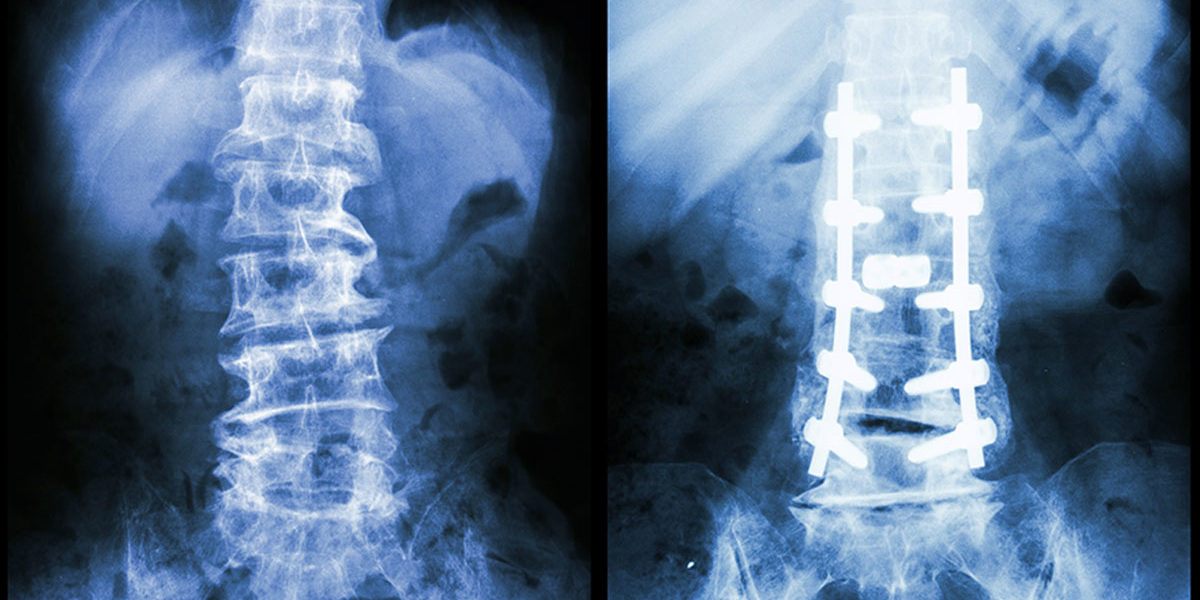
In the US alone, over 300,000 spinal fusion surgeries are performed every year to correct for fractures, deformations, or spinal instabilities. These surgeries are often performed by inserting a pedicle screw into the damaged vertebrae to increase the strength of the fusion. These screws are most often used in cases where the bone in the surrounding area is already weak, which decreases the likelihood of success in the surgery. Essentially, pedicle screws are used in damaged bones to increase their strength, in turn increasing the likelihood of success in a high-risk patient.
However, a common issue with pedicle screws is loosening over time which often results from the body rejecting the screw or gradual fatigue over time. Either way, if loosening happens, the patient needs more treatment or even further surgery. This can be costly or painful and it puts the individual at further risk of death or infection.
Solving the Screw Loosening Problem
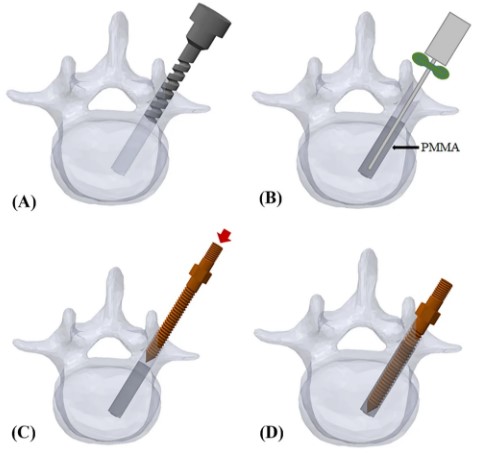
In the last twenty years, efforts have been made to reduce screw loosening by using bone cement augmentation. This is the process of including polymethylmethacrylate (PMAA), or bone cement, in the bone with the pedicle screw to strengthen the surrounding bone and overall, increase the strength of the pedicle screw. The cement acts to manually increase the density of the weakened bone allowing the screw to get more of a hold. Think of trying to screw into a piece of wood versus drywall; while it may be harder to get in at first, a screw in a piece of wood is much more difficult to pull out than one in drywall.
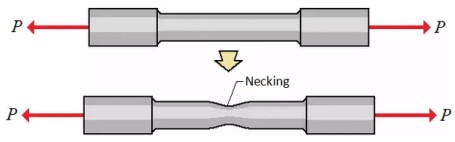
From now on, the pullout strength used to measure the effects of cement augmentation represents the force, P, when the screw and bone break. This is analogous to the figure shown left, except instead of the “dog bone” sample it is a human vertebra and screw being pulled apart.
This thinking was supported in 2004, when Cook, et all. compared the pullout strength of a pedicle screw with PMMA and to one without PMMA in human vertebrae. After testing, the screw with the PMMA was roughly 250% stronger than the screw without the PMMA. This discovery eventually led to PMMA being adopted in the medical community.
In 2021, Jung Son, et al. followed 187 patients as they went through spinal fusion surgery some with cement augmentation and others without. They confirmed researchers’ earlier beliefs that patients undergoing cement augmentation had improved outcomes than those who did not. This was especially prevalent in patients with high-risk factors such as old age, osteoporosis, or autoimmune disease.
A critical component of cement augmentation as a whole is the risk of leakage. If the cement leaks outside of the bone during surgery, it can spread to other areas of the body and lead to a pulmonary embolism or neurological deficits. In the study conducted by Jung Son, there were no complications from cement leakage indicating that when done carefully, cement augmentation can be implemented with limited to no added risk to the patient.
Looking Ahead
The effectiveness of bone cement augmentation is evident both in research and in real-world use, but there is still work to be done to further reduce the risk of cement linkage and improve the methods of inserting the cement. Huge leaps have been made in this area, but there are always improvements to be made when a person’s life is at stake.