Prosthetic devices have been an option for limb-different individuals for thousands of years. Over the centuries, there have been countless discoveries that have led to the modern prosthetic leg. Today’s customary prosthetic leg is comprised of two main components: the socket and the device itself. The socket is often made of carbon fiber and is molded to the contours of the user’s residual limb. This socket is directly connected to the device itself, which includes an ankle and possible knee joint depending on the length of the limb. The socket serves as the connection point between the user’s residual limb and the prosthetic leg.
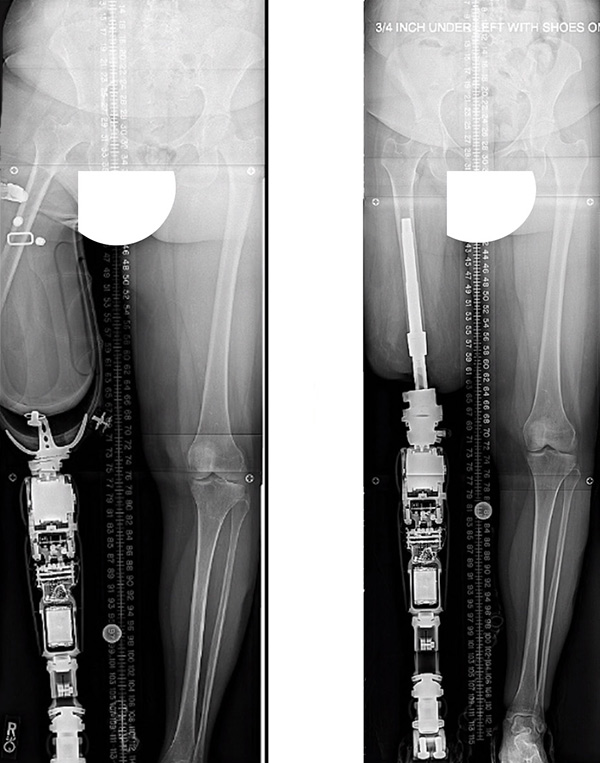
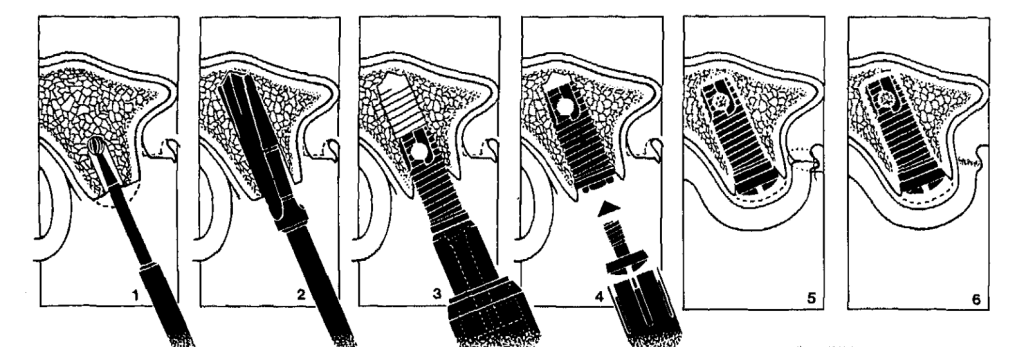
Unfortunately, the common socket option is not compatible for all limb different individuals. Whether it be that the residual limb is too short for the socket to create a comfortable connection, there is a risk of skin breakdown due to rubbing of the socket, or the need for increased proprioception to aid in walking, an alternative to the socket is needed. This is where osseointegrated prosthetic legs come into play. Simply put, an ossiointegrated prosthetic (OP) device offers a connection to the prosthetic device through a screw threaded into the bone of the residual limb. One side of the screw is placed into the bone of the residual limb (oftentimes at the time of amputation), while the other side of the screw extends through the muscle, fat and skin of the limb to be used as an attachment for the device itself.
The first successful OP device was implanted in May of 1990. This procedure would not have been possible without the decades of research that contributed to this success. Two of the most important discoveries that led to this successful surgery are the discovery of titanium as a viable biocompatible material and the extensive work behind osseointegrated tooth implants often used in dentistry.
One of the most basic requirements for a successful OP device surgery is using a material that will interact well with the patient’s internal environment. Today, these devices are made of titanium, a known biocompatible material, thanks to the discovery of Dr. Brånemark. Astonishingly, his discovery was one of chance! While studying the blood flow in rabbits, he observed that the titanium fixtures which he was using in his research had tightly adhered to the bone of the rabbit. He theorized this was because the body had created a connection to this material. This was revolutionary because prior to this discovery, it was a commonly held belief that the body would reject any foreign object introduced into it. This finding opened the door for extensive research into the feasibility of medical implants which inevitably became a cornerstone for OP devices.
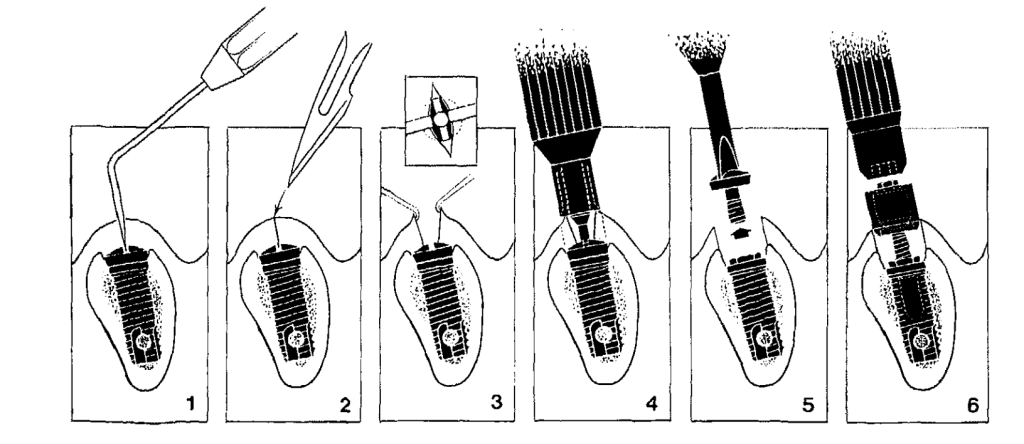
A second key study was conducted by R. Adell, U Lekholm et al. and observed the outcomes of hundreds of patients who were recipients of osseointegrated tooth implants over 15 years. This study outlined a surgical technique that served as a foundation for the surgical plan for osseointegrated legs. Similar OP legs, this surgery is completed in two phases. The first surgery inserts the screw into the bone, and the second one is to attach the fixture which will protrude out of the skin. A critical discovery of this study was that the patient needed to heal from the first surgery without any load on the implant to allow the bone to create a secure connection with the screw.
Thanks to the findings of Dr. Brånemark, R. Adell, U. Lekholm, et al., and hundreds of others in the field, the development and successful surgical application of OP devices have become a reality for patients worldwide. This technology is still in its infancy and has the potential for countless advancements including stronger defense against infection after surgery and improved design to better suit each individual patient. OP devices have paved the path towards increased mobility and independence for it’s users for the past several decades and will continue to be a representation of opportunity for years to come.
Featured Image from: Pexels