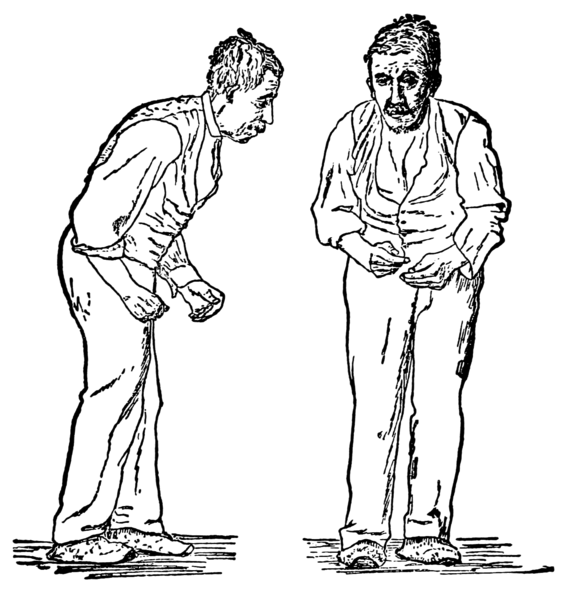
Parkinson’s disease is the second most common neurodegenerative disease with 90,000 Americans being diagnosed every year. Parkinson’s is a difficult disease to detect; there are no blood or lab test to diagnosis it. Diagnoses are symptom based. Parkinson’s patients often do not know they have the disease until after having dealt with it for years. Some of the early symptoms such as facial masking (lack of facial expression), small handwriting, or speaking softly do not directly point to a Parkinson’s disease diagnoses. A patient comes in with tremors, muscle rigidity, poor balance, and slowed movements and are then assumed to have Parkinson’s disease. If their symptoms improve with medication, the diagnosis is confirmed. Biomechanics is a useful tool in the evaluation of the progression of the disease as well as its continued treatment.
One use of biomechanics in the treatment of Parkinson’s disease is the analyses of the patient’s gait. Gait is the manner that a person walks, and there is “healthy” gait and problematic gait. Biomechanics, more specifically, kinematics, can be used to determine how far a person’s walking pattern deviates from the “healthy” gait. Kinematics is the study of motion through things like position, velocity, and acceleration. In the paper “The biomechanics of motor control of gait in Parkinson’s disease,” the many papers looking at gait biomechanics are compared. It was found that those with Parkinson’s had a gait that significantly deviated from the normal person’s gait. Their stride length and speed was decreased, which decreased their overall walking speed. This causes the patient to shuffle their feet, which increases their risks of falling. One factor they looked at when analyzing gait kinematics was whether or not the subject was on medications for the disease. In studies where the patients were on medication, there was not a significant increase in stride length or speed compared to without medication. All of these studies only compared straight line walking, which is not representative of what someone with Parkinson’s needs to navigate on a day to day basis. The paper suggests that further research of Parkinson’s gait needs to include things such as stopping and turning to provide more applicable results.
Biomechanics is also used to look at posture, especially during the gait cycle, and the postural instability that those with Parkinson’s develop. Postural instability can lead to injuries and falls, which become more dangerous as people age. In a paper by Molly A. McVey et. al , different biomechanical variables, such as center of pressure (the point in the foot that undergoes the most force when walking) and joint kinematics (joint motion) are evaluated to see if there is connection between them and the patient’s postural instability. Further research is needed, but the study showed that Parkinsons affects movement significantly. With how hard Parkinson’s is to diagnose, further research in this area may provide some different factors to look at for diagnoses, and diagnoses will hopefully start to happen earlier on in the disease progression.
Gait and posture are only two of the the many things biomechanics can be used to evaluate and treat in Parkinson’s disease. As Parkinson’s disease largely affects motor skills, biomechanics is a useful tool in seeing how movement is restricted or uncontrolled as the disease progresses. As patients try more treatments, medications, and therapies, biomechanics can provide data to show improvement or decline to give doctors a cohesive look of the patients health.
Further Reading:
Rigidity in Parkinson’s disease: evidence from biomechanical and neurophysiological measures
The biomechanics and motor control of gait in Parkinson disease
Early biomechanical markers of postural instability in Parkinson’s disease
