COVID-19 vaccinations reduce the risk of infection and have the potential to ensure life returns to normal. Everywhere you turn someone is talking about which vaccine they have received: Pfizer, Moderna, Janssen, AstraZeneca… But what is the difference? How do the different types of COVID-19 vaccinations protect us? And does it matter which vaccine you receive?
Continue reading “COVID-19 Vaccines: Helping You Combat One Spike Protein at a Time”Tag: COVID
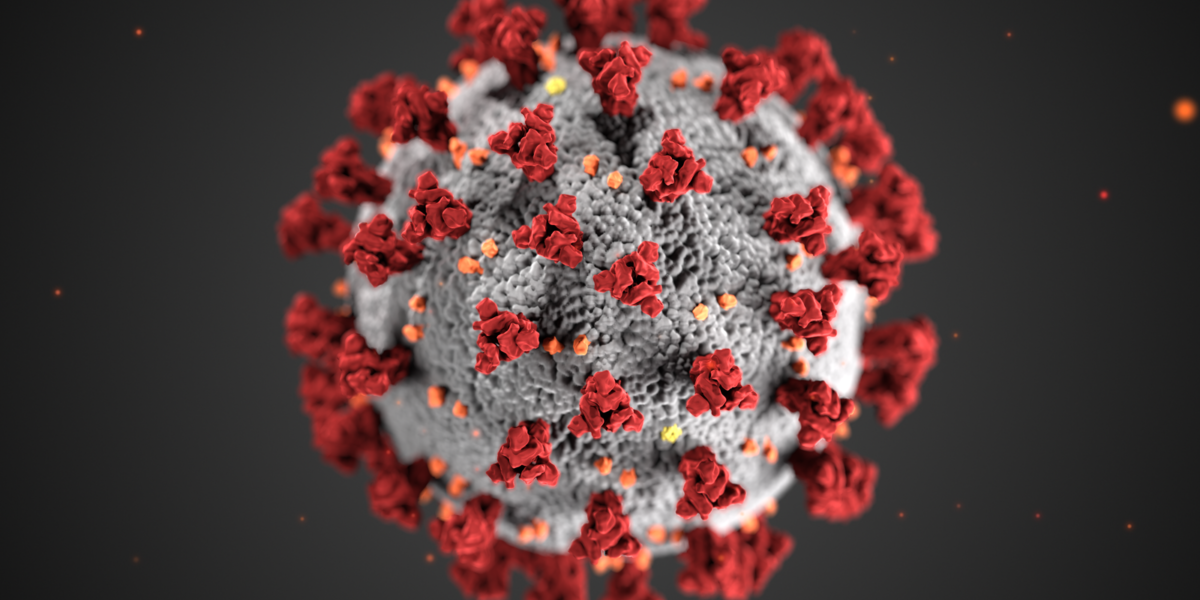
the novel coronavirus: how an invisible invader halted the world
Last year the world changed. With modifications to daily life such as wearing masks and attending class online, a lot of what was common became uncommon. More severely, millions of deaths globally shook the world. All of this change and devastation can be attributed to a coronavirus variant that was shockingly good at two things… 1.) Stability outside of cells 2.) Breaching the lower respiratory tract. A few questions must be understood as to why this virus is so effective in its affinity towards destruction. First, How does COVID-19 penetrate a cell? How does COVID 19 replicate? Finally, why is COVID-19 able to survive outside of a cell so well?
Continue reading “the novel coronavirus: how an invisible invader halted the world”