You might think that breathing in our sleep should come naturally – if breathing and sleeping are both physiologically necessary, then we must be able to do them simultaneously right? Unfortunately, almost a quarter of middle-aged American men and nearly 10% of women suffer from sleep apnea, a chronic condition characterized by repeatedly stopping breathing while sleeping. The clinical symptoms seem rather benign – snoring, sleepiness, fatigue during the day or other issues sleeping. However, by far the most dangerous aspect of this disease is that it puts patients at increased risk of high blood pressure, stroke, coronary heart disease, as well as occupational and/or automobile accidents. Over the last several decades, a variety of therapy options have been studied to treat this condition, ranging from drugs to masks to surgery.
One of the earliest documented therapy options is using protriptyline to treat obstructive sleep apnea. Protriptyline is an anti-depressant drug that was used for its ability to clear airway obstructions during sleep; however, it did not gain significant popularity due to its adverse effects including cardiac complications and limited demographics for whom it would be an appropriate treatment.
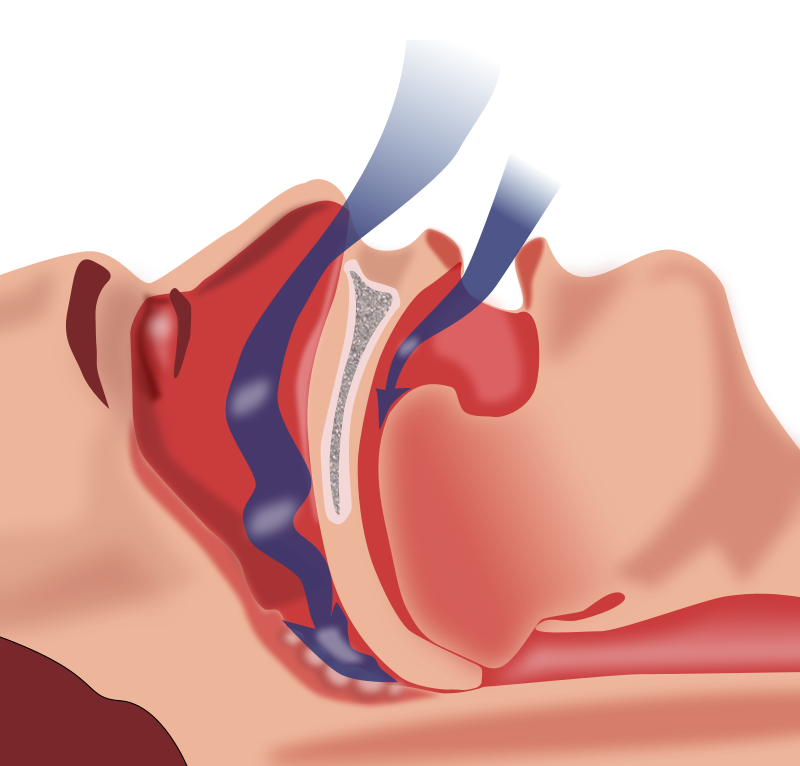
The next treatment discussed was altering sleep positions for patients suffering from sleep apnea. A seemingly simple idea, a study determined that laying on the back significantly increased the severity of sleep apnea. Interestingly, the difference in severity between back and side sleeping positions was most noticeable in healthy, non-obese patients. The authors believe that lying on the back causes tissues of the throat to obstruct the trachea and prevent smooth airflow during breathing, as shown in the image below, which would explain why obesity can exacerbate sleep apnea.
Multiple non-invasive devices were also studied, including oral appliances, sleep posture alarms, and positive airway pressure devices. Oral appliances can either protrude the lower jaw or restrain the tongue; both aim to restructure the upper airway (mouth, trachea, etc.). Sleep posture alarms were suggested to train patients to sleep on either side, rather than on their backs. Positive airway pressure devices (Bi-PAP, CPAP) are the most commonly used treatment for sleep apnea currently; they maintain a consistent air pressure flowing into the mouth to ensure the airways do not collapse during sleep.
The final treatment studied was nocturnal supplemental oxygen (NSO), which involves increasing the concentration of oxygen in the air inhaled while sleeping. However, a study comparing use of a CPAP with use of NSO found that CPAP treatment was far more effective at decreasing the patients’ blood pressure and still proved effective in patients already taking blood pressure medication.
Overall, the best method for treating sleep apnea is dependent on the patient and his or her underlying conditions. Changes in sleep posture could greatly enhance the sleep quality of a moderate case of sleep apnea; CPAP would be ideal for someone who can easily tolerate the mask and does not frequently move in his or her sleep. Each of these demographics makes it difficult to define one optimal solution for treating sleep apnea, but the variety of available treatment options provides hope for those patients who suffer from this chronic illness.