COVID-19 vaccinations reduce the risk of infection and have the potential to ensure life returns to normal. Everywhere you turn someone is talking about which vaccine they have received: Pfizer, Moderna, Janssen, AstraZeneca… But what is the difference? How do the different types of COVID-19 vaccinations protect us? And does it matter which vaccine you receive?
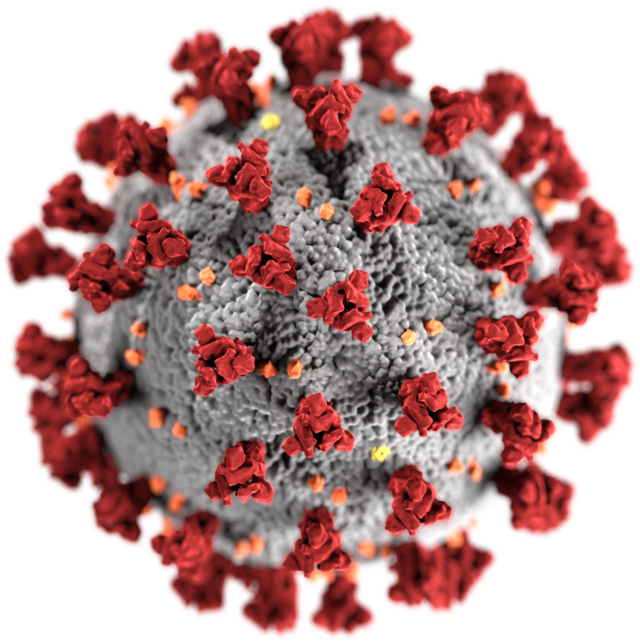
To start off, it is important to understand how coronavirus enters our cells: spike protein. Spike proteins are visually the spikes protruding from the spherical coronavirus and what bind to our cells to transmit the RNA virus (a code for COVID-19), enveloped inside the coronavirus, to our cell’s cytoplasm (the area inside a cell excluding the nucleus). The spike proteins fuse to our cell membrane (the outside of the cell) and are the target for researchers and vaccine developers.
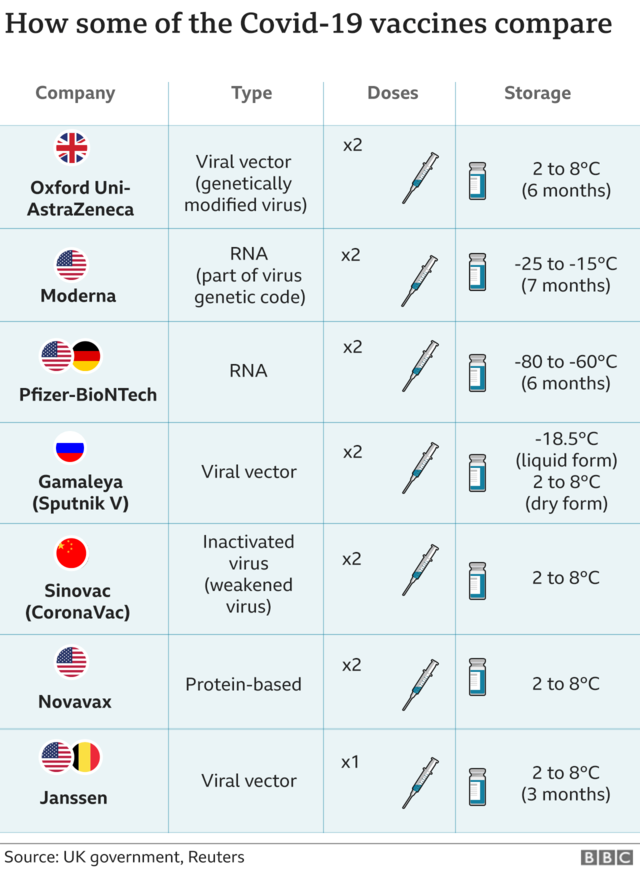
There are various types of vaccines that stop the spike proteins from fusing to our cell membrane, however, the two main types of vaccines used in the United States are mRNA vaccines and viral vector vaccines. Pfizer and Moderna are mRNA vaccines, while Janssen and AstraZeneca are viral vector vaccines. Both types of vaccines have the same goal: create antibodies to bind to spike proteins to block the spikes from attaching to and infecting healthy cells.
The Pfizer and Moderna vaccines use messenger RNA technology to deliver genetic code to our cells to instruct how to make the SARS-CoV-2 spike protein. mRNA is very fragile thus it is encapsulated in something called lipid nanoparticles (LNPs) in order to reach the cell. LNPs increase translatability and stability to ensure mRNA’s delivery to the cell. When the mRNA vaccine is delivered to our cell it breaks free of the LNPs.
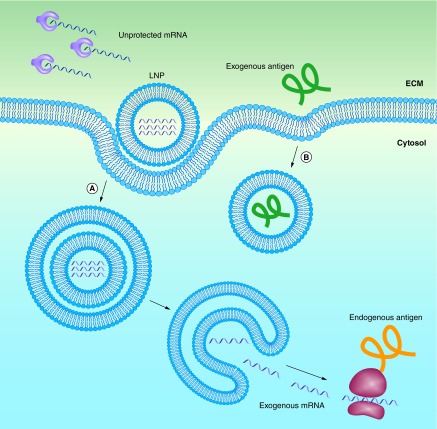
After the mRNA is released from the LNPs, the cell begins making spike proteins. The spike proteins then trigger an immune response to begin producing antibodies. Ultimately, the antibodies latch onto the coronavirus’s spikes making the virus unable to latch onto other cells.
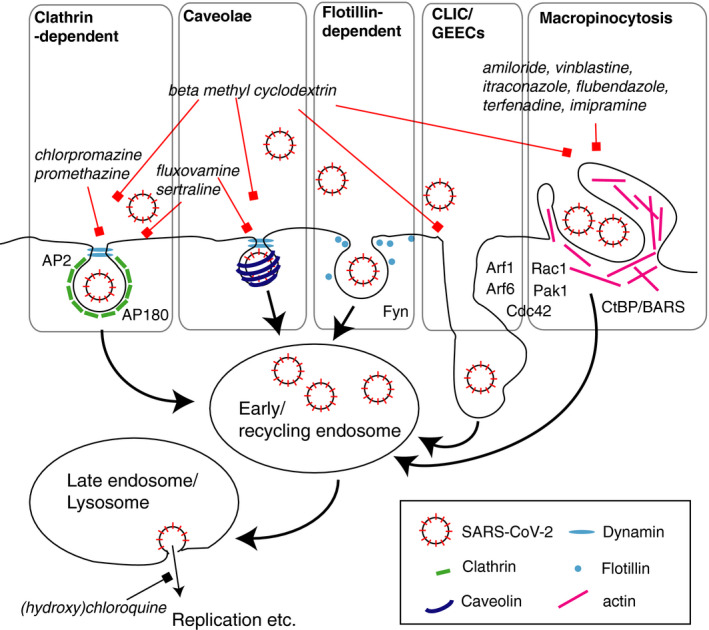
The Janssen and AstraZeneca vaccines incorporate viral vector vaccine technology. The viral vector is a genetic code that creates an instruction manual for human cells to produce the SARS-CoV-2 spike protein transported into the body by a harmless virus called an adenovirus. The adenovirus acts as the delivery system for this important DNA code and helps the body to trigger an immune response.
The vector vaccine attaches onto proteins on the cell’s surface and the adenovirus is pulled into the cell. The main difference between the mRNA vaccine and the viral vector vaccine is that the DNA in the adenovirus of the viral vector vaccine must travel into the cell’s nucleus in order to be transcribed whereas the mRNA vaccine remains in the cytoplasm throughout the process. From there viral vector vaccine acts very similar to mRNA vaccines—once the DNA is transcribed into mRNA, the mRNA leaves the nucleus and the cell begins assembling spike proteins.
Further research is being completed to determine exactly how COVID-19 vaccines enter the cell. However, endocytosis is thought to be the answer based on previous vaccine knowledge. Endocytosis is a cellular process in which something is brought into the cell by engulfing it in a vesicle (small fluid bubble). In mRNA vaccines, the LNPs take advantage of the natural process of endocytosis. The LNPs are engulfed in a bubble, triggering a reaction that allows the nanoparticle to enter the cell and eventually release the mRNA.
Overall, both the mRNA and viral vector vaccinations are great options each with their own unique design to produce antibodies and stop coronavirus from latching onto our cells.

Featured image cropped from Pfizer-BioNTech COVID-19 vaccine (2020) A by Lisa Ferdinando licensed under CC BY 2.0.