Have you ever wondered how a woodpecker is capable of banging its head against a tree so furiously without seriously injuring itself? The impact of a woodpecker’s beak with a tree can exceed speeds of up to 6 meters per second and occur over 12,000 times a day.These kinds of numbers are what allow woodpeckers to smash through trees to get to those tasty bugs that live inside.
Continue reading “How much wood can a woodpecker peck? The Science Behind a Woodpecker’s Anatomy”Month: September 2019
Put One Foot in Front of the Other? It’s Not that Easy
From Christmas movies to pop songs to motivational posters, we are encouraged to keep putting “one foot in front of the other.” While the sentiment is inspiring, recent studies show that there is a lot more to the seemingly simple task of walking than this phrase would suggest. Understanding this is especially important for balance and mobility after an injury or as people age.
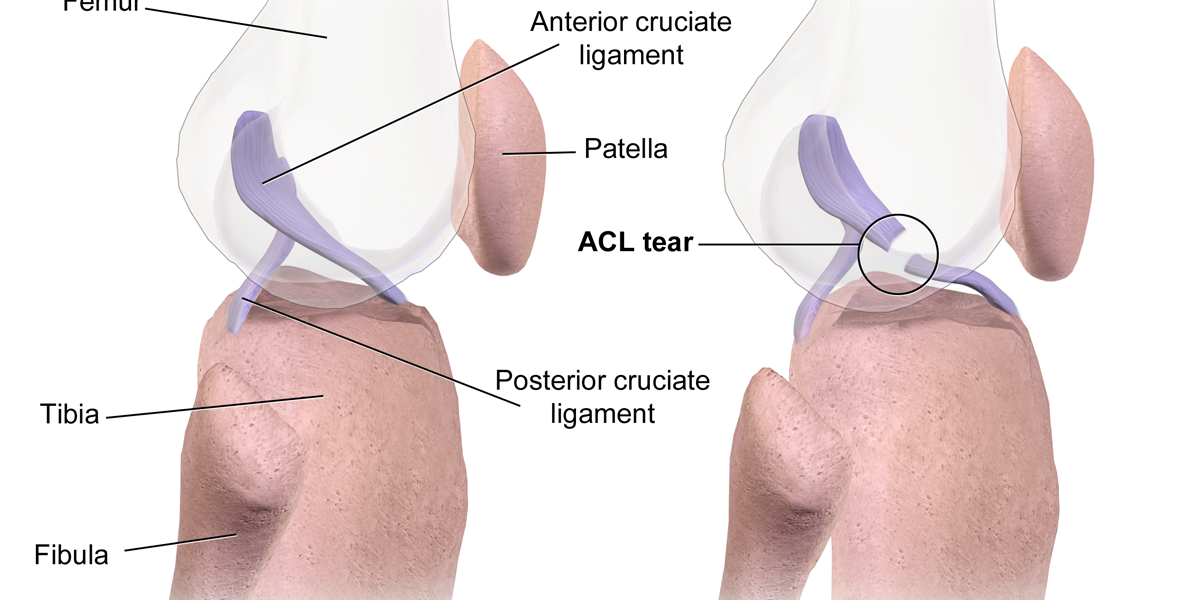
Continue reading “Put One Foot in Front of the Other? It’s Not that Easy”ACL Reconstruction: Which Option Is Best For You?
200,000 ACL injuries occur each year, and ACL reconstruction is the 6th most performed surgery in the United States, so to come back bigger, faster, and stronger, the right recovery path is critical.
Continue reading “ACL Reconstruction: Which Option Is Best For You?”Patellar Tendinitis: The Kryptonite of Jumping Athletes
Volleyball is a sport of quick movements. For hitters, one of the most common movements in the game is the jump, whether that be to block or to hit. Although a higher vertical leads to improvement in game performance, it can increase the risk of developing a serious injury that affects many volleyball players: patellar tendinitis. This condition is associated with pain and tenderness directly below the knee cap that is especially apparent during explosive, jumping movements. But what exactly causes this condition? And what can be done to remedy it?
Continue reading “Patellar Tendinitis: The Kryptonite of Jumping Athletes”Biomechanics of Pitching: Pushing Limits on the Shoulder and Elbow
Aroldis Chapman of the New York Yankees holds the Guinness World Record for the fastest recorded baseball pitch at 105.1 MPH; a record that has held for almost a decade. Why has no one been able to top his record? — An answer to this question may be found in the biomechanical limits of the human shoulder and elbow during the throwing motion.
Continue reading “Biomechanics of Pitching: Pushing Limits on the Shoulder and Elbow”The Spinal Fusion that Reignited a Legendary Career
Can you imagine being the best player in the world at a certain sport and one day, aggravating an injury that not only put your athletic career in doubt, but also did not allow you to do normal daily activities? This is the challenge that faced Tiger Woods.
Continue reading “The Spinal Fusion that Reignited a Legendary Career”Skeletal Support Seekers’ Success (So Far)
Bones break, and broken bones need time to heal, or regrow. Fans of J.K. Rowling’s Harry Potter series are quite familiar with the concept of bone repair, as Harry is once required to drink a Skele-Gro potion to magically (and painfully) regrow his arm bones overnight. Now, as fantastic as it would be to completely fix broken bones in a few hours, modern medicine has not yet discovered that secret of the Wizarding World; however, several treatments have been developed in attempts to speed the rate of fracture repair as well as increase the comfort of the patient (take that, Skele-Gro).
Continue reading “Skeletal Support Seekers’ Success (So Far)”Ways to Prevent and Treat a Common Annoyance: Headaches
Headaches can range from a mild annoyance to a debilitating condition that results in the inability to complete simple daily tasks. Odds are you have experienced a headache since about 50% of the population has suffered some type of headache. While there are many different variables that may have triggered it (injury, stress, chemical imbalances, etc.), the resulting symptoms are always negative. Scientists have been investigating what causes different types of headaches in hopes that they can help people prevent their occurrence and mitigate their symptoms.
Continue reading “Ways to Prevent and Treat a Common Annoyance: Headaches”Medical Marvel: Robotic exoskeletons enable those with spinal cord injury to walk again
A fall off of her horse in 2007 caused Claire Lomas to lose all function in her legs. In 2012, she completed the London Marathon, all 26.2 miles. Robotic exoskeletons can literally get people back on their feet shortly after a spinal cord injury occurs, but how exactly do these medical devices not only supplement but restore human performance? What does the future look like for robotic exoskeletons and those with paralysis?
Continue reading “Medical Marvel: Robotic exoskeletons enable those with spinal cord injury to walk again”